By Akshata J. Balghare
In January 2020, University Health Services at the University of California, Berkeley (UCB) shared an informational handout on its Instagram page that focused on “managing fears and anxiety” about Coronavirus Disease 2019 (COVID-19). With an intent to offer mental health tips and resources, the infographic identified a handful of “normal reactions” that people might experience during the crisis. Surprisingly, the post listed “xenophobia” as one of the normal reactions, defining xenophobia as “fears about interacting with those who might be from Asia and guilt about those feelings.” This post received an extensive backlash for normalizing xenophobia, which hurts Asian, as well as other foreign, populations. The Health Services Center later deleted the post and issued an apology. UCB’s fiasco brings to light how risk communicators can unintentionally encourage acts that may sound biased, exclusionist, or even racist while also undermining their real message.
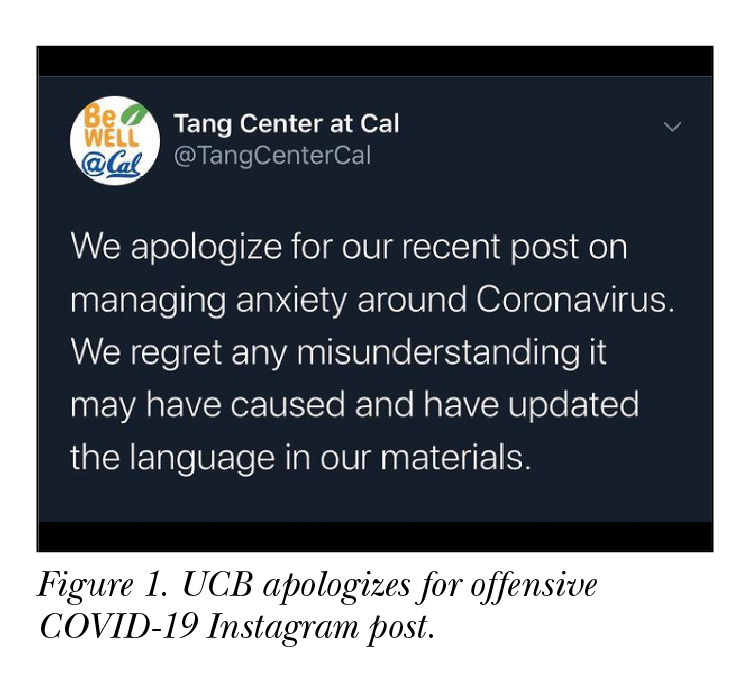 Communication experts Reynolds and Quinn (2008, 16S) mention that the responsibility of risk communicators is to construct messages “that will reduce illnesses, save lives, and maintain societal structures.” A message like the one from UCB, however, disrupts beneficial societal structures and stimulates unwanted behavioral changes. The World Health Organization and U.S. Centers for Disease Control and Prevention communication guidelines are based on building a relationship of trust between communicators and audiences, a trust that tells the public that they should believe the communicator and take risk measures per the received information (Abraham 2011). In that case, is UCB asking audiences to trust that xenophobia is normal and that the university is not unintentionally harming their own foreign population? Their message could have resulted in UCB damaging its trust with its foreign population and those who care about them.
Communication experts Reynolds and Quinn (2008, 16S) mention that the responsibility of risk communicators is to construct messages “that will reduce illnesses, save lives, and maintain societal structures.” A message like the one from UCB, however, disrupts beneficial societal structures and stimulates unwanted behavioral changes. The World Health Organization and U.S. Centers for Disease Control and Prevention communication guidelines are based on building a relationship of trust between communicators and audiences, a trust that tells the public that they should believe the communicator and take risk measures per the received information (Abraham 2011). In that case, is UCB asking audiences to trust that xenophobia is normal and that the university is not unintentionally harming their own foreign population? Their message could have resulted in UCB damaging its trust with its foreign population and those who care about them.
COVID-19, which originated in China, spread globally, and people of Chinese or Asian descent have been harassed and treated differently, leading to a pandemic of xenophobic behavior and fearmongering around the world. “In the United States, as the infection emerged, more than 1,000 media reports of racism and xenophobia against Asian Americans were recorded between January and February 2020” (Kandil CY 2020, as cited in Ng 2020, 1158).
Such xenophobic attitudes were also detected previously during the 2003 SARS outbreak. For example, Chinese immigrants in New York were stigmatized and blamed by other residents in the community in response to the uncertainty that surrounded SARS at the time (Eichelberger 2007, as cited in Wirz et al. 2018, 2602). Both Ding (2007) and Sontag identify that xenophobic propaganda have always depicted immigrants as bearers of disease (Sontag 2003, as cited in Ferguson 2019, 144).
Some of this xenophobic behavior could have resulted from the way COVID-19 information was communicated. In the case of global epidemics, there is a high chance of risk communication messages harming vulnerable populations. Rhetoric such as referring to COVID-19 as the “Chinese virus,” “Wuhan virus,” and the “kung-flu” has been promoted by some US leaders, “providing the necessary oxygen to fan the flames of hate and discrimination against members of the targeted communities” (Ng 2020, 1158). Additionally, “many reports on COVID-19 also include a picture of an Asian person wearing a mask” (Gee, Ro, and Rimoin 2020, 955). Wardman (2008, 1620) warns us that “even when risk communication has been implemented in good faith and according to plan, it seems that the possibility for ‘effective’ risk communication is far from certain and that in some instances it may in fact do more harm than good.”
A few missteps can trigger loss of trust in the expert’s ability to communicate about the crisis, leading to unexpected and highly undesirable outcomes for minority and marginalized populations (Vaughan and Tinker 2009, S324). For example, a message that attacks and blames the Chinese population can have spillover effects to other communities, causing members of other Asian subgroups (e.g., Vietnamese, Koreans, Japanese) to also become targets of anti-Chinese discrimination (Gee, Ro, and Rimoin 2020, 954). Gee, Ro, and Rimoin (2020) point out that people experiencing discrimination might opt to hide out and not get tested or treated, which could skew COVID-19 data and our understanding of the disease. Consequently, such individuals may suffer through the disease by avoiding treatment owing to the fear of discrimination and hostility.
This contradicts what we want to achieve as risk communicators, and so we must experiment with ways to construct a reasoned dialog involving different stakeholders, especially during pandemics when multicultural stakeholders are involved. Ding (2013) suggests that experts consider the public’s emotions, attitudes, and cultural values to make better risk policies, communicate more effectively about risk measures, and produce more desirable outcomes, especially during transcultural risk communication.
In addition to the abovementioned strategies by Ding, we should consider the following: “What elements of a message or a communication context are likely to enhance or diminish the persuasive effect of a message? What elements of the message are remembered, and which ones trigger changes in opinions or attitudes?” (Renn 1992, 484). IEEE ProComm (2020) recently posted an article discussing how choosing active verb forms and emphasizing personal responsibility by using the right subjects can provoke the public to take personal actions as a means of addressing the problem. Their article “Language Choices in Times of Crisis” recommends saying “‘you’ and ‘we’ are spreading the virus” because those words underscore the reader’s role in the spread, emphasizing personal responsibility.
This suggests that when communicating about a risk to the public, considering “agency” and the way of addressing agents is central. However, even though we consider agency, we may face challenges crafting appropriate messages around risk using language and rhetoric that fits within the expectations of all cultural populations. In the case of UCB, the message does not address all of its agents because it only speaks to people who are not Asian/Chinese, and it subtly attributes blame to the Asian/Chinese population for the disease. In this way, the message ignores the role of non-Asian populations in the spread of COVID-19 on UCB’s campus.
While COVID-19 harms some populations more than others based on their access to healthcare or privilege to socially distance or stay home, we should not forget that “we’re” all at risk, and COVID-19 can infect anyone regardless of their race, religious belief, gender, or sexual orientation. As technical communicators, we must design risk messages using language that is free of stereotypes, cultural insensitivity, sexism, or any sort of discrimination. Our role is of symbolic analysts and user advocates when communicating risk information, and we possess the ability to create user knowledge in risk communication processes (Grabill and Simmons 1998, as cited in Ding 2013, 127). Thus, we must be mindful of the messages we construct as risk communicators because our messages create crisis management knowledge for the public. Accordingly, our messages must consider suitable agency, be credible and ethical, and address agents in ways that motivate them to take the right actions.

AKSHATA BALGHARE (Akshata.Balghare@ttu.edu) is a PhD student of Technical Communication and Rhetoric at Texas Tech University. She has experience working as a technical editor for engineering-focused research articles and is currently teaching technical writing as a graduate instructor. Her research interests include intercultural communication, healthcare communication for minorities in the United States, and engineering and scientific communication.
The Student Perspectives column provides insights, experiences, research, and more from students across technical communication. We’re proud to introduce new voices, inject new ideas, and give the practitioners of tomorrow a platform to begin publishing their thought leadership today! Column editor Ryan Weber teaches technical communication at the University of Alabama in Huntsville and hosts the podcast 10-Minute Tech Comm. Contact him at rw0019@uah.edu to submit or pitch a column idea.
References
Abraham, Thomas. 2011. “Lessons from the Pandemic: The Need for New Tools for Risk and Outbreak Communication.” Emerging Health Threats Journal 4 (1): 7160.
Ding, Huiling. 2007. “Rhetoric of a Global Epidemic: Intercultural and Intracultural Professional Communication about SARS.” PhD diss., Purdue University.
Ding, Huiling. 2013. “Transcultural Risk Communication and Viral Discourses: Grassroots Movements to Manage Global Risks of H1N1 Flu Pandemic.” Technical Communication Quarterly 22 (2): 126–149.
Ferguson, Elizabeth Deane. 2019. “Decolonizing Epidemics: Power Structures That Define, Name, and Frame Medical Disasters.” PhD diss., George Mason University.
Gee, Gilbert C., Marguerite J. Ro, and Anne W. Rimoin. 2020. “Seven Reasons to Care About Racism and COVID-19 and Seven Things to Do to Stop It.” American Journal of Public Health 110 (7): 954–955.
IEEE ProComm. 2020. “Language Choices in Times of Crisis: Wordsmithing our Response to COVID-19.” 4 April 2020. https://procomm.ieee.org/language-choices-in-times-of-crisis-wordsmithing-our-response-to-covid-19/.
Nature. 2020. “Stop the Coronavirus Stigma Now.” 7 April 2020. https://www.nature.com/articles/d41586-020-01009-0?fbclid=IwAR2e-EYtv9NYZrmekhUeymvxwb5NlQG78LGa3_lpEIUFRx3JOzqpCfzVE20.
Ng, Edmond. 2020. “The Pandemic of Hate Is Giving Novel Coronavirus Disease (COVID-19) a Helping Hand.” The American Journal of Tropical Medicine and Hygiene, 102 (6): 1158–1159.
Renn, Ortwin. 1992. “Risk Communication: Towards a Rational Discourse with the Public.” Journal of Hazardous Materials 29 (3): 465–519.
Reynolds, Barbara, and Sandra Crouse Quinn. 2008. “Effective Communication during an Influenza Pandemic: The Value of Using a Crisis and Emergency Risk Communication Framework.” Health Promotion Practice 9(4): 13S–17S.
Vaughan, Elaine, and Timothy Tinker. 2009. “Effective Health Risk Communication about Pandemic Influenza for Vulnerable Populations.” American Journal of Public Health 99 (S2): S324–S332.
Wardman, Jamie K. 2008. “The Constitution of Risk Communication in Advanced Liberal Societies.” Risk Analysis: An International Journal 28 (6): 1619–1637.
Wirz, Christopher D., Michael A. Xenos, Dominique Brossard, Dietram Scheufele, Jennifer H. Chung, and Luisa Massarani. 2018. “Rethinking Social Amplification of Risk: Social Media and Zika in Three Languages.” Risk Analysis 38 (12): 2599–2624.