doi: https://doi.org/10.55177/tc885177
By Keshab Raj Acharya
ABSTRACT
Purpose: This study was designed to better understand how mobile health applications (mHealth apps) designed in the Global North (GN) are perceived as usable, empowering, and persuasive by users, particularly healthcare practitioners, in the context of a Global South (GS) country.
Method: This article employed an online survey of users of a mHealth app that was designed and developed in the GN for global use. Survey participants included healthcare practitioners from a GS country and the survey was administered by snowball sampling method.
Results: Eighty-three survey responses from healthcare practitioners in Nepal were coded into three broad categories: user experience and mHealth apps, localized usability and mHealth apps, and persuasive design and mHealth apps. Their relationships and connections are examined within these categories.
Conclusion: From a user empowerment perspective, understanding the interest, motivation, and concerns of end-users is vital to the development and implementation of mHealth apps, especially in the low- and middle-income healthcare contexts in which healthcare practitioners have limited resources. Culturally sustaining localized UX approaches should be adopted to create usable, empowering, and persuasive mHealth apps for use in resource-constrained cultural settings in the GS.
KEYWORDS: mHealth apps, Localization,User empowerment, Persuasive design, Global South and Global North
Practitioner’s Takeaway
- Technical communicators as healthcare practitioners need to pay attention to cultural aspects prevalent in users’ sites in developing and evaluating UX of health-related tools for user empowerment and persuasion.
- Localized usability studies can provide insight into and act as a driving force for designing usable, empowering, and persuasive care-related tools that meet the needs and expectations of healthcare practitioners from other cultures.
- In designing such tools, practitioners in the Global North need to consider users in the Global South by addressing users’ localized usability expectations and needs so the North–South divide can at least be reduced, if not eliminated.
INTRODUCTION
The widespread use of smartphone technology and mobile health applications (mHealth apps1) has significantly impacted global healthcare delivery systems. In addition to reducing existing patient care and treatment barriers such as provider workload, skills shortage, linguistic and cultural barriers, and geographical obstacles, mHealth apps have opened new avenues for improving health outcomes (Fiordelli et al., 2013). Aside from supporting traditional healthcare research, they are widely used as persuasive tools for clinical decision making, information management, and medical education and training (Sezgin et al., 2017). Such apps have constantly been utilized to manage chronic diseases, fitness, and wellness, as well as to build a participatory health culture that allows users to make informed decisions by promoting their well-being, preventing diseases, and assisting them with managing chronic illnesses (Adepoju et al., 2017; Pokhrel et al., 2021; Welhausen & Bivens, 2021).
Several mHealth apps, including Medscape, Epocrates, PEPID, UpToDate, and Doximity, are available for healthcare practitioners to enhance clinical practices. As mobile devices become more common in expanding global healthcare settings, apps like these are in high demand and being developed quickly (Wallace et al., 2012). These apps must meet user needs and expectations, especially in resource-constrained settings or contexts with “limited access to, or reduced availability of, resources” ranging from “robust bandwidth to electricity to literacy” (Rose, 2016, p. 433). In fact, usability is key in the adoption of mHealth apps (Gagnon et al., 2016)—i.e., individuals must be able to use such apps to achieve a specific purpose.
Scholars in healthcare fields have assessed the effectiveness of mHealth apps in the Global South (GS)2 (e.g., Bhatta et al., 2015; Osei & Mashamba-Thompson, 2021; Pokhrel et al., 2021). Scholars in technical communication (TC) also observe how users experience such apps and attempt to identify users’ functional and productive usability concerns (Welhausen & Bivens, 2021), suggesting that such tools be designed to address the UX needs in a complex healthcare system (Kirkscey, 2020). However, TC lacks research of localized usability implementation in contemporary health technologies—how Global South (GS) healthcare practitioners perceive, use, and experience these emerging digital spaces generated in the Global North (GN).
This article seeks to address this research gap by investigating the extent to which localized usability is implemented in an mHealth app designed in the GN to support healthcare practitioners around the globe. More specifically, the article addresses concerns related to localized usability for user empowerment and persuasion by analyzing survey data collected from Medscape app users (i.e., healthcare practitioners) in Nepal, a small landlocked country between China in the north and India in the south. Nepal was chosen because many of the author’s colleagues who are healthcare practitioners in Nepal expressed dissatisfaction with the design of northern mHealth apps like the case app in this study—the Medscape app.
For this case study, localized usability is defined as the degree to which local practices and values are incorporated into health-related tools (such as mHealth apps, medical devices, medical software, and print or online care-related documents) for a user from another culture (Acharya, 2018; Esselink, 2000; Sun & Getto, 2017). The results from this study can inform TC practitioners and researchers about how localized usability of mHealth apps can improve health efficiency and effective use of care-related tools, including mHealth apps, for problem solving and decision making in resource-constrained situations.
ABOUT THE MEDSCAPE APPLICATION
Developed by WebMD (medscape.com), an American corporation and leading online publisher of health and well-being information, the Medscape app was developed for global use. As a comprehensive resource for medications, diseases, and medical calculators, the app features the drug database, blogs, a checker for drug interactions, a directory of pharmacies and physicians, and more (Lazakidou & Iliopoulou, 2012). The app provides:
- Immediate clinical answers, including prescription and over-the-counter (OTC) drugs, herbals, and supplements
- Latest medical and health information, including the Food and Drug Administration (FDA) approval alerts and expert commentaries
- Consultations with experts, exclusively for healthcare practitioners
- Medical education activities including mobile courses for continuing medical education (CME) credits
- Personalized Activity Tracker to monitor educational progress and credits earned.
(WebMD LLC, 2022)
Both Android and iOS users can download the app for free but they must register. More than 5 million users have downloaded the app from the Google Play store (Google Play, 2022).
Users have unlimited access to the entire Medscape network of sites and services for free. The app provides information on more than 8,500 prescriptions and OTC drugs, herbals, and supplements (WebMD LLC, 2022), and its version (9.2.10 as of this writing and 9.2.9 in November 2021) (Apple Store Preview, 2021) and database are updated regularly (Ming et al., 2016). The app can be used to ask questions, share cases, learn from others, and interact with a global community of healthcare practitioners. As the app includes a drug reference tool with current prescribing and safety information, it provides users with recent global medical and health issues. As for the clinical updates, the app is the most recommended mHealth app that offers free CME activities and medical news (Ming et al., 2016).
This app was chosen because the app was designed and developed within the GN context; it is used by healthcare practitioners in Nepal (Chaudhary et al., 2019); and both Android and iOS users can download the app for free. The app offers news from the Medscape website while keeping healthcare practitioners informed about the latest medical and health information (Phillips & Thornbory, 2014); it gathers recent medical research articles into a single, easy-to-use platform for healthcare practitioners worldwide.
LITERATURE REVIEW
Recent usability research and practices in TC have highlighted our field’s needs to critically examine usability in relation to promoting social justice (Acharya, 2018; Jones & Williams, 2017); user empowerment (Ladner, 2015; Opel, 2014; Walton, 2016); user engagement (Roy, 2013); accessibility (Hitt, 2018; Oswal, 2019); and user advocacy (Jones et al., 2016; Martin et al., 2017; Rose, 2016). In addition, scholars have addressed usability with regard to sociocultural issues, including translation and multicultural user experience (UX) (Cardinal et al., 2020; Gonzales & Zantjer, 2015); cultural sensitivity (Sun & Getto, 2017); and context of use (St.Amant, 2017a). Scholars also recognize the growing need to create technical materials or tools that address user expectations in international contexts (e.g., Gu & Yu, 2016; Saru & Wojahn, 2020).
Localization is the process of designing an information tool to satisfy the needs of a specific target market or country (Hoft, 1995). Localization has been described as the process of adapting content to address linguistic and cultural expectations of specific cultures in specific contexts (Batova & Clark, 2015). User localization involves focusing on strategies and activities that users adopt when they communicate to meet their culturally-specific needs and expectations (Sun, 2012). Developers, understanding user-localization, can design technologies to meet user needs in localized contexts (Gonzales & Zantjer, 2015). When designing healthcare tools for healthcare practitioners across culturally situated local contexts, localization efforts should target users’ sociocultural systems, behaviors, and environment of use. Thus, localization entails contextualizing health-related tools to improve the lives of users, including underserved and underprivileged healthcare practitioners in the GS.
As global markets for technical materials expand, developing medical and health tools that meet the localized usability expectations of other cultures is becoming increasingly important (Acharya, 2019; St.Amant, 2017a, 2017b). Given the global expansion of technical communication, researchers have stressed the need for developing localized medical and health materials to improve the lives of multicultural users (e.g., Batova, 2010; St. Germaine-McDaniel, 2010; Zhu & St.Amant, 2007). To be more effective, health-related tools should be designed to support users’ knowledge and experiences from other cultures. One way of responding to the needs of local users in various contexts is designing such tools with those users as co-designers who can offer “valuable user input” in the locally situated cultural context (Andrews et al., 2012, p. 139). Collaborating with local users means learning from them, in addition to sharing their frustration, pain, and discomfort with the designers (Acharya, 2018). Partnering with users has many advantages, such as a better understanding of just futures and how to work collectively to build those futures (Dombrowski, 2017). In essence, designers can engage in socially just design for inclusion and user empowerment through user participatory design practices—to conduct their work ethically.
Designers of healthcare tools, including mHealth apps, should strive to design not just for healthcare practitioners but also with them: to establish a direct relationship with users as co-designers and, as a result, adopt an effective design approach and allow democratic and participatory engagement (Ehn, 1992; Spinuzzi, 2005). Working closely with users by implementing the participatory civic engagement model allows designers to reflect on users’ needs and desires through an iterative process.
Individuals’ contexts for utilizing healthcare tools can differ per culture, and these differences have important implications for design (Acharya, 2019; St.Amant, 2017b). To accommodate expanding multicultural and multilingual global health contexts, conventional design approaches might need to be modified and improved. For these reasons, many researchers in TC have developed contemporary design frameworks to understand the importance of culturally localizing content (Batova & Clark, 2015; St.Amant, 2021; Sun, 2012, 2020). St.Amant (2017b) proposed the script-prototype approach for the study of UX with care-related tools across national and cultural boundaries. Because scripts influence the way audiences conceptualize messages, they can significantly impact communication in healthcare settings (St.Amant, 2021).
When designing for global audiences, Sun (2020) has developed the “culturally localized user experience (CLUE)” approach for global engagement and empowerment, which is renamed “culturally localized user engagement and empowerment (CLUEE)”—the CLUE2 (CLUE-Squared) approach (p. 6). Although the CLUE approach helps designers integrate different design aspects into products for locally situated cultural contexts, the CLUE2 framework sees design as a mode of sociocultural inquiry as well as a force for social activism (Sun, 2020). Adopting the CLUE2 approach can enable app developers to design mHealth applications for user empowerment by bridging “cultural differences with design intervention” in an international context (p. 7).
Culturally sustaining localized UX approaches are critical in the design of care-related tools to ensure improved healthcare quality and safety. However, many tools are designed without such approaches and thus are difficult to use and have poor user interfaces (Zhang et al., 2003). Essentially, localized UX approaches involve creating interfaces, including mHealth apps, that are usable (effective and efficient), empowering (accessible and supportive), and persuasive (credible or trustworthy) to culturally diverse users in our increasingly globalized world.
Informed by Fogg’s (2003) theory of persuasive technology, interactive design can change users’ attitudes and behaviors—in a word, persuasion. For Fogg, persuasion is a noncoercive attempt to change another person’s attitude or behavior, or both. Fogg (2003) presented seven attributes for developing persuasive technology tools that can change users’ attitudes and behaviors:
- Reduction: to simplify the task sequence required to achieve a desired objective
- Tunneling: to guide a user through activities with specific instructions
- Tailoring: to design information that is compatible with the users
- Suggesting: to suggest actions to the user at the right moment and context
- Self-monitoring: to enable users to track their own behavior
- Surveilling: to observe users overtly to increase a target behavior
- Conditioning: to rely on providing reinforcement (or punishments) to the user.
As persuasive tools, mHealth applications can influence attitude and behavior changes by increasing self-efficacy and providing tailored information (Fogg et al., 2009).
Self-efficacy describes how users believe in their ability to successfully act in a domain, and tailored information provides content that is relevant to their needs. Tailored information can lead to a greater change in behavior and attitude (Dijkstra et al., 1998; Strecher, 1999).
METHOD
This case study examines the extent to which the Medscape app was designed for user empowerment and persuasion in the GS context. Case studies allow researchers to explore in-depth single or multiple units of study (Creswell, 2009), as cases are bound by time and activity, and researchers gather detailed data by employing methods such as interviews or surveys (Stake, 1995). Case studies have proven useful in TC in comprehending complex systems and embodied UX during the development and testing of healthcare tools (Arduser, 2018; Kennedy, 2018; Kirkscey, 2020).
This case study was guided by the following research question: In the development and UX evaluation of health-related materials or tools for user empowerment and persuasion, how can TC practitioners address the needs of healthcare practitioners in the GS context?
To address this research inquiry, I employed a survey to elicit responses from a specific pool of Medscape app users—especially healthcare practitioners—in Nepal. After gathering surveys, I completed qualitative analysis by coding responses.
In surveys, questions are pre-defined to collect information from people (Dillman et al., 2014), with the goal of maximizing response rates and accounting for nonresponse bias (Fink, 2017).
An online survey was employed because of its benefits, including lower cost, faster response time, flexibility, ease of data entry, and control over the format (Granello & Wheaton, 2004) and because it may allow researchers to gain access to populations that otherwise might not be possible (Wright, 2005).
I incorporated snowball sampling through social media: to recruit participants who are not accessible or who do not know the researcher (Marcus et al., 2017; Naderifar et al., 2017) and to expand the participant pool by having participants connect me with potential participants.
Potential users of the Medscape app were contacted via email, phone, and social media messaging platforms; the two inclusion criteria were healthcare practitioners, including medical students, in Nepal and users of the Medscape app for at least one month.
For this IRB-approved study, I designed and administered 25 survey questions using the Qualtrics survey instrument (see Appendix). I am unsure how many potential participants saw the invitation, so a response rate cannot be determined. A total of 88 participants took part in this study, but three did not complete the survey and two did not meet the inclusion criteria; therefore, the analysis is confined to 83 participants’ responses as data sources.
Using an Excel workbook, the data corpus was unitized (segmented for analysis), sampled (selected an acceptable number of texts to analyze), and validated (used a consistent coding system) for emerging and recurring themes (Boettger & Palmer, 2010). Informed by Flick’s (2018) coding procedure, I utilized the stages of open, axial, and selective coding. Although open coding was performed to generate conceptual categories, axial coding was done to refine theme categorization. Using selective coding, the core category was determined, relating it with other categories derived from axial coding. I did not employ secondary raters because I was not attempting to quantify the data, but to draw connections between the data points. Though I acknowledge that this may be a shortcoming, additional raters are no guarantee of reliability or validity (Armstrong et al., 1997).
I examined each response and considered its implications at a larger scale, seeking to avoid bias. At times, different categories appeared to be similar but were, in fact, quite different. If a phrase or term fit into more than one category but had nothing else to accompany it, I kept that content in the category with related terms or phrases. In so doing, I grouped related phrases in their own category that otherwise would be scattered throughout the results without context for analysis.
RESULTS
To address my research question, I analyzed and coded participants’ survey responses to derive themes and grouped them into three thematic categories: user experience and mHealth apps, localized usability and mHealth apps, and persuasive design and mHealth apps.
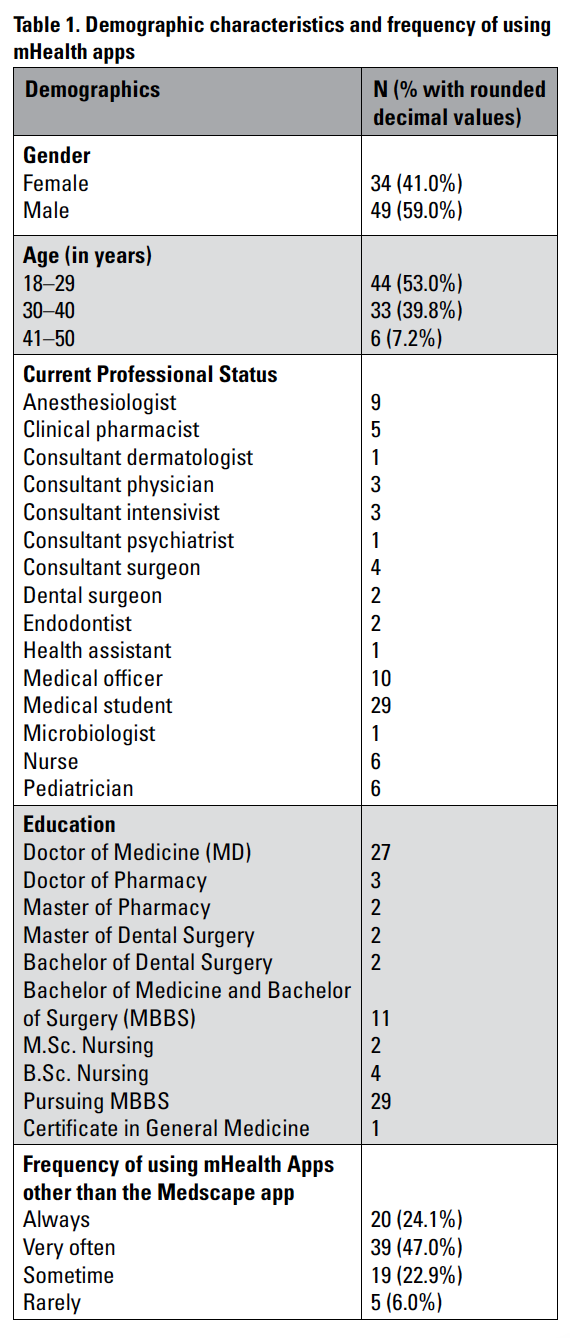
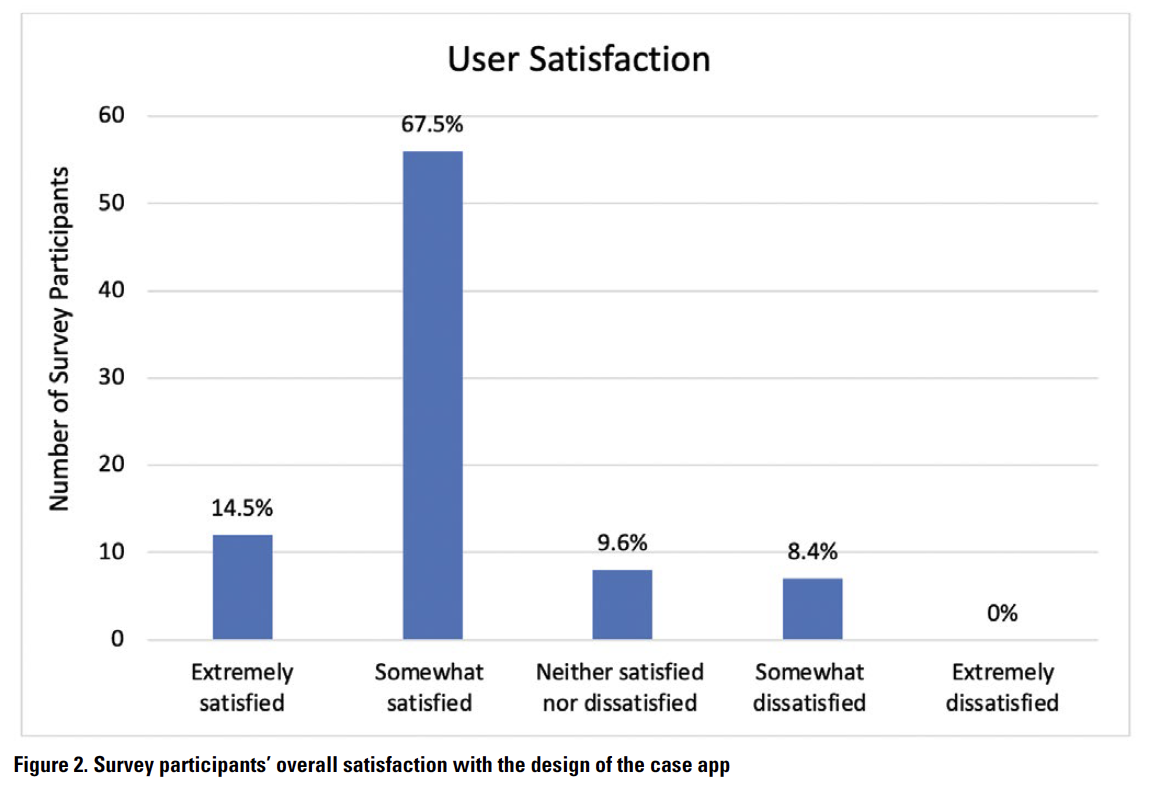
The first step was to analyze the collected data to gain a better understanding of the study participants’ demographics. Of 83 respondents who indicated their gender, 34 (41%) were female and 49 (59%) were male (Table 1). Respondents reported ages from 18 to 50 years. Among the participants, 44 (53%) were younger than 30 years, 33 (39.8%) were younger than 41 years, and six (7.2%) were 41–50 years.
Participants’ current occupations varied widely. Twenty-nine were medical students pursuing an MBBS degree, and 54 were healthcare practitioners from different departments, including anesthesia, dermatology, critical care, psychiatry, surgery, pathology, dentistry, pediatrics, pharmacy, and ophthalmology. Nine nurses and 10 medical officers also took part in the study.
As for other mHealth apps, 20 participants (24.1%) always utilize them, 39 (47%) very often, 19 (22.9%) sometimes, and five (6%) rarely. Although nine participants (10.8%) mentioned using a locally designed mHealth app called DIMS Nepal, 23 (27.7%) reported using UpToDate, which was designed and developed in the GN for worldwide use. Five participants (6%) indicated that they use only the Medscape app. Thirty participants (36.1%) utilize this app many times a day, six (7.2%) use it once a day, 19 (22.9%) many times a week, 18 (21.7%) once or twice a week, and 10 (12.1%) use the app on a weekly basis. These data support Chaudhary et al.’s (2019) findings that the Medscape app remains popular among healthcare practitioners in Nepal.
User Experience and mHealth Apps
Enhancing UX requires understanding the ways technical tools are designed for persuasion and how the choices they offer position a user to act in the context of use (Lauer & Brumberger, 2016). Health-related tools designed with the user in mind increase the likelihood of adoption and the impact of actual use (Alsswey et al., 2020; St.Amant, 2017a). To better understand users’ perspectives on the design of information in the case app, participants were asked if the information was designed to meet their needs and expectations in their cultural contexts. Nineteen (23%) participants strongly agreed on the design of information for the healthcare practitioners who need to use it, 51 (61.4%) moderately agreed, and nine (10.8%) responded as neutral, but four (4.8%) participants expressed some disagreement with the design of the information (Figure 1). One participant stated, “I would like to say that this app does not provide information in short and in a clear manner.” Implicitly indicating the localized usability issue associated with the design of information, one participant expressed:
Information should be presented in ways that we could use it based on our geographical location. For example, if the app prioritizes information based on diseases endemic in a particular geographical region, it could be easy and simple for us to use the app during a public health crisis in our country.3
 Similarly, two participants mentioned the vagueness of information and one noted that it is “too difficult to find out what is needed in the critical or urgent care situation.” Another expressed dissatisfaction regarding the design of information: “I cannot find all the information I need on a country-by-country basis.” What works in one culture may not work in another.
Similarly, two participants mentioned the vagueness of information and one noted that it is “too difficult to find out what is needed in the critical or urgent care situation.” Another expressed dissatisfaction regarding the design of information: “I cannot find all the information I need on a country-by-country basis.” What works in one culture may not work in another.
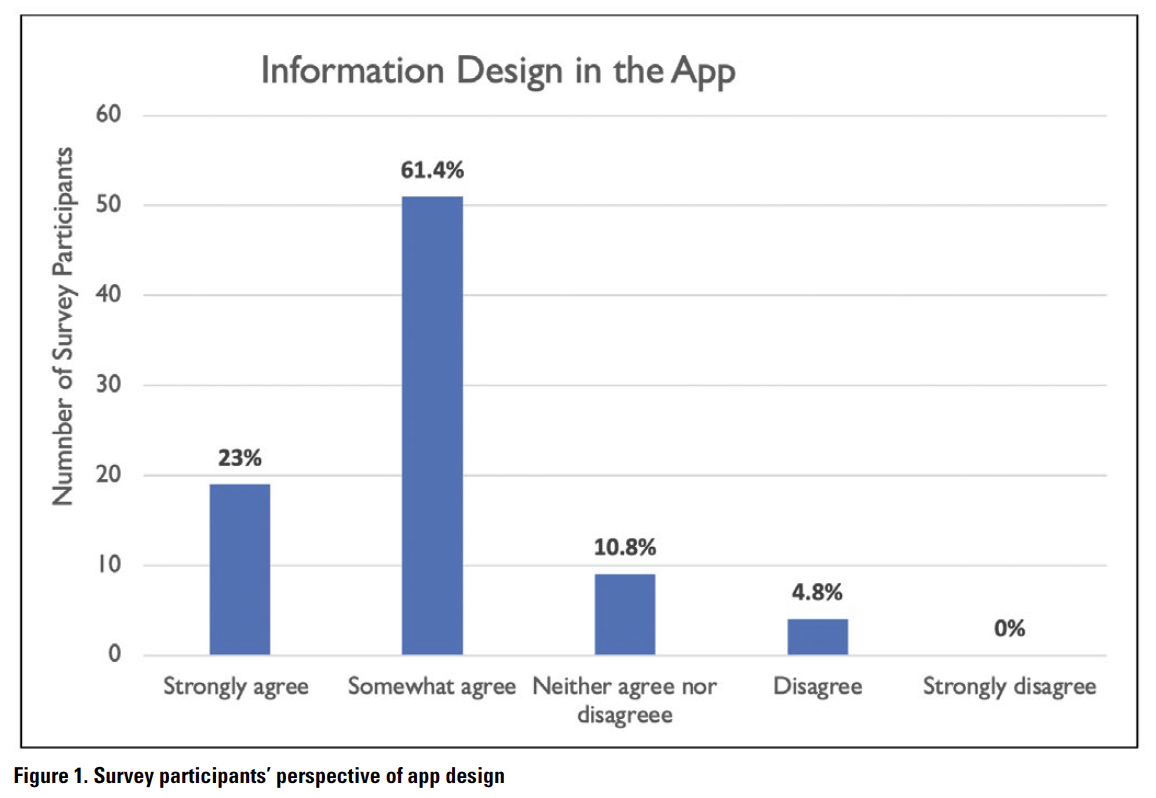
Because user satisfaction is a key attribute of usability (Barnum, 2011; Nielsen, 1993), participants were asked how satisfied they were with the case app’s performance and design in their immediate environment. Twelve (14.5%) participants were extremely satisfied with the app, 56 (67.5%) were moderately satisfied, eight (9.6%) were neutral, and seven (8.4%) were somewhat dissatisfied (Figure 2).
 Though most participants were relatively satisfied, the main concerns of user discontent are the requirement to log in and the lack of up-to-date information. One participant mentioned:
Though most participants were relatively satisfied, the main concerns of user discontent are the requirement to log in and the lack of up-to-date information. One participant mentioned:
The app is not updated with the latest classifications of drugs, and it does not include some newer classification of drugs. I am a little bit concerned with the information about Drug-Drug Interaction. Information about the pharmacokinetics of drugs is somewhat lacking.
Similarly, another participant expressed dissatisfaction: “Sometimes the app does not work when needed. It gets too slow at times.” Thus, when creating mHealth apps as persuasive tools for healthcare practitioners in the GS, developers in the GN need to pay attention to both organizational visions for information design and an action plan for achieving it for localized usability and user empowerment.
Localized Usability and mHealth Apps
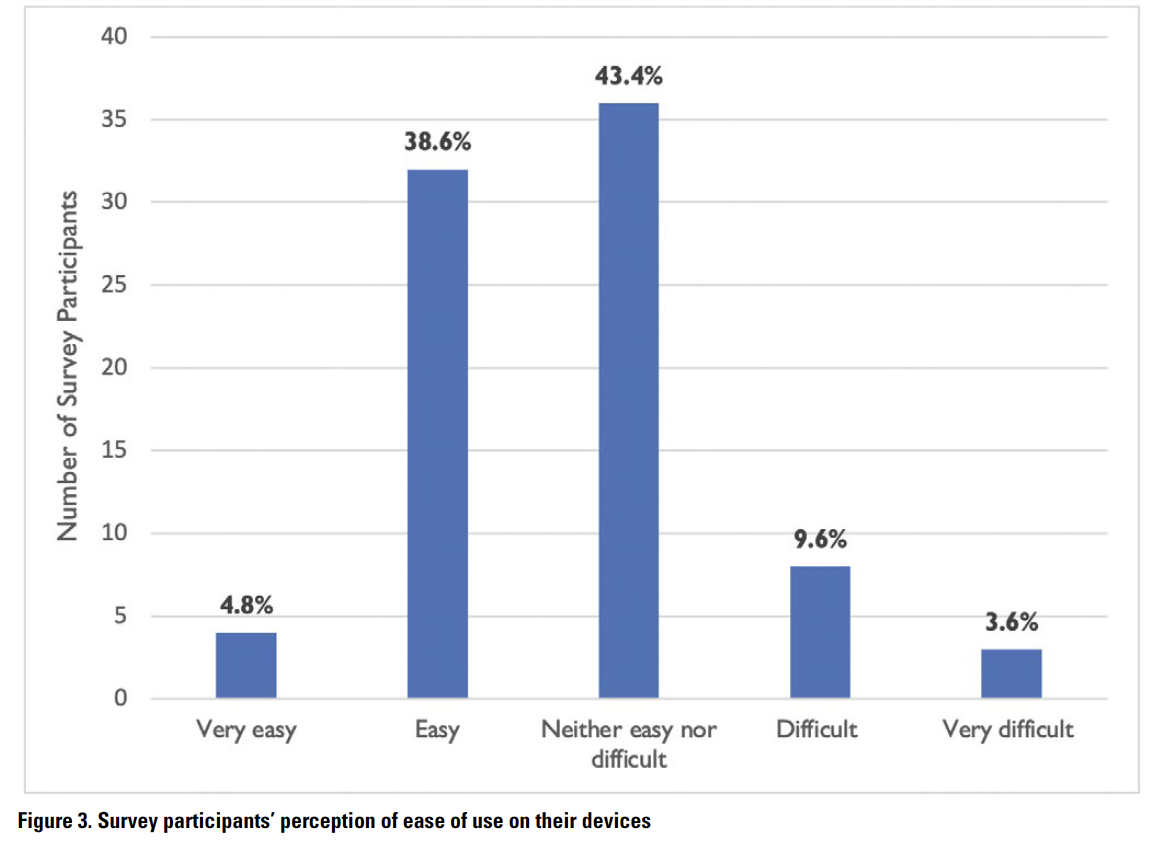
mHealth apps can play a significant role in supporting healthcare practitioners in southern low- and middle-income countries by changing the standards of healthcare services and opening new opportunities (Osei & Mashamba-Thompson, 2021; Pokhrel et al., 2021). As part of the localized usability implementation for effective healthcare services, participants were asked about the installation and operation of the case app on their devices. Thirty-two participants (38.6%) found it easy, 36 (43.4%) were neutral, and eight (9.6%) found the setup process rather difficult (Figure 3). Four (4.8%) participants mentioned that the app was easy to set up, whereas three (3.6%) rated it as very difficult (Figure 3). Regarding the app’s functionality, nine participants (10.8%) reported that the app crashed frequently on their phones, 41 (49.4%) had a moderate view of the issue, 26 (31.3%) rarely faced this problem, and seven (8.4%) had no such issues. Considering whether participants preferred the Medscape app over the Medscape website or both, 59 participants (70.1%) preferred the app, whereas seven (8.4%) favored the website; 17 participants (20.5%) selected both, stating that “the website is easy to navigate,” they do not have “enough memory on [their] phones” to download the app,” and that they “mostly use PC” because “it is much easier to look up more information on the website.” One participant noted that it was “easy to open more than one page simultaneously on the website.”
 Participants reported various reasons for using the app by selecting all applicable options. Although 50 participants (65%) utilized the app to find evidence-based information for effective patient treatment, 24 (28.9%) used it to provide immediate care and health support. Likewise, 49 participants (59%) considered the app a persuasive source of health-related information and 38 (45.8%) indicated its use for making quick decisions in critical care situations.
Participants reported various reasons for using the app by selecting all applicable options. Although 50 participants (65%) utilized the app to find evidence-based information for effective patient treatment, 24 (28.9%) used it to provide immediate care and health support. Likewise, 49 participants (59%) considered the app a persuasive source of health-related information and 38 (45.8%) indicated its use for making quick decisions in critical care situations.
In discussing how the case app was designed for users, especially healthcare practitioners, from other cultures, one participant emphasized the importance of having detailed information over the app’s attractiveness: “I do not think app designers need to make it attractive for users because we mostly use this app for getting health and medical information. Inclusions of all recent updates would make this app more reliable.” Indicating the issue related to localized usability implementation in the app, another participant stated:
To make it more user-friendly, the app should keep its free subscription and consider summarizing key findings in a catchy way. App designers can make it evidence-based by incorporating the major impactful recent clinical trials or system reviews. Other features such as “drug dosing for specific patients or populations” should be added to the app.
The development of mHealth apps with persuasive features that address specific concerns of users, particularly healthcare practitioners, in the GS context can lead to increased localized usability. In short, the presence or absence of a single design feature can have a significant impact on the usability and persuasiveness of an mHealth app in a different cultural context.
Persuasive Design and mHealth Apps
As mHealth apps are gaining more popularity for promoting beneficial behaviors, their design and functionality become increasingly important in persuading healthcare practitioners to use them (Shati, 2020). Beneficial behaviors, in my case study’s context, relate to healthcare practices and activities. Because credibility or reliability is critical for the design of persuasive systems (Fogg, 2003), design flaws can easily result in irreversible losses of perceived source reliability in health technologies or tools.
To better understand GS healthcare professionals’ perception of credibility when using the case app, participants were asked if they found the information credible. Twenty-five participants (30.1%) strongly agreed, 52 (62.7%) moderately agreed, and six (7.2%) were neutral. Despite some participants’ concerns associated with information reliability, the results show that the case app was generally perceived as a credible source of information: “This app is very credible, easy to use, and can be operated when the internet is available.” However, concerns about the app’s credibility include a lack of up-to-date and detailed information for users in specific localities: “The app does not provide up-to-date information as quickly as other apps like UpToDate. It also does not provide detailed information about many topics for healthcare workers like us in Nepal.” The lack of updated information regarding current medical advances, as discussed by another participant, raises concerns about the app’s credibility in the GS context:
Not all medicines are included in the app. Broader information in the app would help us find information accurately in countries like Nepal. Information about new medicines should be available immediately in the app so that we can know what is going on in our field around the world. This also increases the app’s credibility.
As these findings imply, providing detailed content information in mHealth applications can boost persuasion and improve UX in the locally situated GS context.
To enhance localized usability for user empowerment and persuasion in the low- and middle-income healthcare context, mHealth app developers in the GN can consider design principles proposed by Fogg—especially reduction, tunneling, and tailoring. Implementing these principles in mHealth app design, however, differs depending upon the app type, as well as the cultural context where it will be used. These three principles are the most studied design principles for persuasion (Al-Ramahi et al., 2016).
Reduction
Reduction tools make “a complex task simpler” by “reducing a complex activity to a few simple steps (or ideally, to a single step)” to achieve certain goals (Fogg, 2003, p. 33). In my case study, 10 participants (12%) complained about having to log in every time to access information. One participant stated, “I hate having to sign in every time using my email and password.” Another participant expressed a similar sentiment: “Do not ask for the username and password again. I forget them every time.” Discussing the lack of specificity of the information in the app, one participant mentioned, “At times, the app provides too vague answers, making it hard to find out the information that I need.”
The app’s usability can be improved by simplifying tasks or reducing unnecessary steps so that app users, especially healthcare practitioners in the GS, can access information quickly and easily.
Tunneling
Adopting the tunneling design principle allows designers to reduce uncertainty by guiding “users through a predetermined sequence of actions or events, step by step, to encourage certain” beneficial behaviors (Oinas-Kukkonen & Harjumaa, 2018). Like reduction tools, tunneling tools aim to increase self-efficacy and facilitate goal completion by sequencing tasks to reduce the user’s cognitive load—the amount of mental effort required to complete a task. Participants also indicated the issues associated with tunneling in terms of guiding users through a set of tasks in a specific order to achieve a goal. As one participant noted, “I think data and information should be kept with references to standard textbooks so that I can consult them if I need.” Another one reported that “information should be organized more effectively, and sections should be summarized and placed in the appropriate location based on user needs, so that users can find, understand, and use them quickly and easily with a minimal learning curve.”
As a result of applying the tunneling principle during the design process of mHealth apps, developers can simplify the overall process by reducing cognitive load on healthcare practitioners and, thereby, improve the localized usability of such apps for user empowerment and persuasion in southern healthcare contexts.
Tailoring
Tailoring is a way of designing information in a system or tool that is compatible with a user’s educational, cultural, and social background. Users are more likely to utilize systems or tools that are tailored to their needs, personalities, usage contexts, and other characteristics (Al Ayubi et al., 2014). Expressing their concerns related to tailoring tools, six participants (7.2%) reported having difficulty connecting to the Internet to access information. One participant noted that “all topics are unavailable when offline, and [that] the app takes up a significant storage space on mobile devices.”
Participants also mentioned the issue of localized usability and user empowerment. One participant suggested “adding more updated videos related to procedures on a country basis” and another mentioned the issue associated with “not being able to download information when needed to use without internet connection.” Participants also complained that they could not access content if they were offline, and that the information was insufficient. One participant said, “Please make all contents available offline and as a pediatrician we need more detail on management part regarding the doses which is sometimes difficult to find even searching on the Internet.” Another participant suggested that “frequently used sections [be] tailored individually.”
These responses highlight two key localized usability issues that are consistent with how another participant stated it succinctly when commenting on what annoys the user about the app: “trade names of drugs available in US/Canada and content unavailable when offline.”
Thus, participants reported a broad range of localized usability aspects to be considered to design usable, empowering, and persuasive mHealth apps for southern healthcare practitioners. Identified usability aspects were related to functionality, accessibility, information design, contents, features, subspecialties, and updates. In essence, understanding the interests, motivations, and concerns of end-users (healthcare practitioners in this case study) is vital to the development and implementation of mHealth apps for user empowerment and persuasion, especially in the low- and middle-income healthcare contexts in which healthcare practitioners have limited resources.
DISCUSSION
Designing mHealth apps from a localized usability perspective is critical to ensuring better health education, care, safety, and wellness in resource-constrained southern healthcare settings. Findings also reveal that northern mHealth apps are widely used in underdeveloped, underserved southern countries like Nepal, indicating the need for adopting more defined, targeted, and streamlined design approaches for user empowerment and persuasion. Design approaches developed in the GN for improving usability may not always work well in the southern cultural context. Because a one-size-fits-all approach to designing mHealth technologies for local use is also insufficient (Ohno-Machado, 2015), healthcare tools should be designed through localization, which should take place at the user’s site and be a joint endeavor between users and developers (Rose et al., 2017).
My findings also support Welhausen and Bivens’ (2021) findings that functional usability considerations remain crucial for users. Also mentioned were specific problems participants encountered when performing or attempting to accomplish certain tasks. Although some participants were concerned about the app’s functionality, others cited issues related to accessibility, insufficient content, missing features, and updates. These findings emphasize the importance of better understanding users’ localized usability experiences, implying that northern designers should collaborate with southern users as co-designers to respond to the contingencies of locally situated southern cultural contexts.
Although numerous possibilities for persuasion can be considered while designing mHealth apps for southern healthcare practitioners, northern designers can consider applying Fogg’s (2003) design principles as important contributors to localized usability for user empowerment and persuasion. (Table 2 provides an example of how persuasive design concepts can be applied to the development of mHealth apps for localized usability in resource-constrained, underdeveloped countries.)
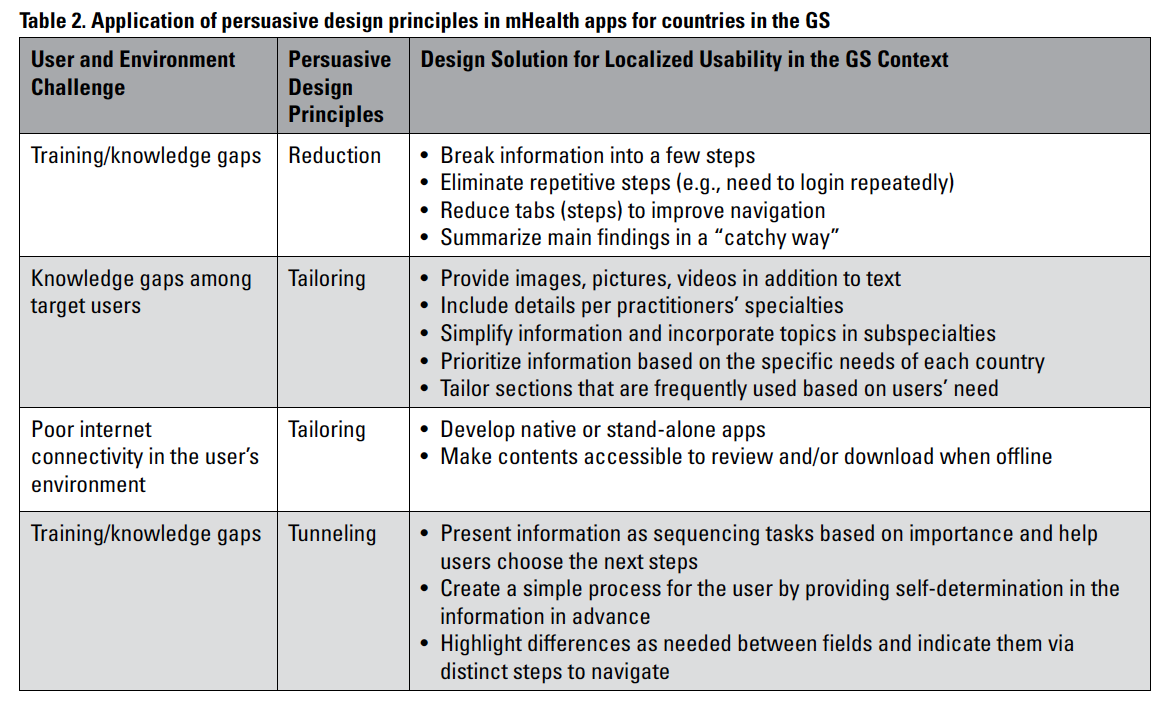
The first column (Table 2) describes the operating environment for such apps in the target culture. Healthcare practitioners in the GS are concerned about knowledge gaps regarding recent trials and videos on new medical procedures. To fill these gaps, practitioners can include multimedia content, with voice instructions, still images, and the latest videos to complement the text content. Many healthcare practitioners in low- and middle-income countries with low-bandwidth internet infrastructure may face additional challenges when using mHealth apps, such as poor internet connectivity. The design solution is to develop native apps using the programming languages of the mobile device or its operating system, allowing the apps to run independently (Budiu, 2016).
Northern designers should acknowledge how such tools can increase users’ abilities or make things easier to perform within the culturally localized southern context. Practitioners can ask key questions to get insight into designing usable, empowering, and persuasive health-related tools from a localized GS perspective:
- Is the tool inclusive and accessible to users, including healthcare practitioners, regardless of their social standing in the target culture where it is used?
- Does the tool enable healthcare practitioners to accomplish their desired goals or objectives with all possibilities in a complex healthcare setting in the GS?
- Is the tool readily comprehensible, usable, and persuasive within the culturally situated local healthcare system in the GS?
- Does it support healthcare practitioners’ localized knowledge systems or existing practices in the target culture?
Answering such questions with “no” suggests that the tool as a persuasive technology can be ethically questionable and perhaps objectionable. The resulting answers can guide TC practitioners if, how, and what kind of supporting skills, knowledge, and practices are needed to incorporate into the design of healthcare tools for multicultural and multilingual users. Practitioners can also use the answers to address localized usability barriers and make users’ tasks less overwhelming within the GS’s complex healthcare systems.
IMPLICATIONS FOR PRACTICE AND RESEARCH
mHealth apps, including the Medscape app, are the most popular medical sources among healthcare practitioners worldwide (Rebedew, 2018). As my findings suggest, healthcare practitioners in the GS use mHealth apps designed in the GN to obtain evidence-based medical and health information, current medical breakthroughs, and detailed information about topics related to health and medicine. In non-Western contexts, healthcare practitioners’ top app choices, as my findings reveal, are native apps and those that provide detailed and up-to-date information. Thus, technical communicators should focus on functionality, practicality, and details when developing persuasive medical and care-related tools for healthcare practitioners in the GS.
As TC spreads globally, understanding another culture’s localized usability expectations requires practitioners to gather data directly by interviewing members of the target culture or conducting focus groups with members of that culture. However, practitioners should be aware that many usability-enhancing “data collection methods developed in the West (such as in-depth interviews, surveys, focus groups, and think-aloud protocols) do not always work well in non-Western cultures” (Baxter et al., 2015). Engaging multicultural healthcare practitioners as co-designers by embracing and developing effective localized user research methods before and during development and UX evaluation of medical and care-related tools can foreground the intentionality of localized design for culturally diverse healthcare practitioners in the increasingly globalized world. To this end, adopting Sun’s (2020) CLUE2 approach and Fogg’s (2003) persuasive design principles, rather than ad hoc methods, can equip practitioners in the GN with a systematic conceptual basis and framework with which to create such tools, including mHealth apps, to engage cultural differences in this global village.
Given the need for addressing medical and health-related activities and practices in different cultural contexts, TC scholars have called for culturally sensitive materials for the targeted user community in the international context (e.g., Hall et al., 2004; St.Amant, 2015). However, questions concerning localized usability for user empowerment and the application of persuasive design principles in mHealth apps for promoting self-efficacy in southern healthcare settings are not well addressed in our field. Conducting more research can, in Sauer’s (2018) words, “offer our field more and better prospects for future prosperity” (p. 370). Building a more equitable and inclusive future starts with understanding users’ needs and expectations, including those of disadvantaged and underrepresented healthcare professional groups from other cultures. So, medical and health research in TC as a field should be directed toward supporting these groups by engaging cultural differences globally. In short, as TC goes global, localized usability research across low- and middle-income healthcare contexts is needed for accomplishing our long-standing commitment to social justice and equity.
LIMITATIONS
As with other research projects, this study has limitations and strengths. The results were based on participants’ self-reported data in one small country in the GS, thus liable for bias in terms of generalizing the results in other heterogeneous contexts across cultures. The survey was limited to a few open-ended questions, so asking more questions would allow participants to reflect on their experiences with the app. Also, further qualitative data could be obtained by interviewing or conducting focus groups, or through ethnographic methods such as contextual observations.
In terms of numbers of apps, users, and investments, the US occupies a very large share of the global mHealth market (“Global mHealth Industry,” 2020). So, a cross-cultural study on the localized usability of the case app between high-income and low-income settings could help designers better understand and address user needs and expectations in the development and UX evaluation of such tools for Western and non-Western multicultural healthcare practitioners in the global context.
CONCLUSION
This study emphasizes the importance and value of localized usability implementation in health-related tools, such as mHealth apps, for user empowerment in the GS. mHealth apps that apply persuasive design principles can achieve a predetermined objective or outcome. As the TC field expands globally, practitioners need to better understand what it means to design persuasive care-related tools for users in non-Western countries, especially those with poor healthcare systems. I call upon TC practitioners in the Global North to empower users in the Global South by addressing users’ localized usability expectations and needs so that the North-South divide can be reduced.
NOTES
- Though what distinguishes a care-related mobile app as a “health app” or a “medical app” is unclear, they can be distinguished by purpose: for reference and information gathering, medical education and training, and wellness and fitness as well as to offer diagnostics and therapeutic assistance (Albrecht et al., 2014). Applications that are designed to diagnose, treat, alleviate, or prevent disease, or that impact the structure or function of the body may be classified as medical apps and subject to FDA regulation (Roth, 2014). Such apps are designed with medical purposes in mind, whereas health apps generally address individuals who are interested in obtaining health-related information for managing health and wellness, including medical education and training, and those who do not turn mobile devices into regulated medical devices or generate patient-specific data (Roth, 2014).
- The GN and GS replace classic descriptors such as “first world versus third world” or “more developed versus less developed” nations in discussing socio-economic differences between those countries that have greater wealth and influence, and those that have less. Countries in the GS have generally less rate of human development, whereas those in the GN have a high index rating (Odeh, 2010). These terms are, however, not geographically absolute because some countries in the southern hemisphere are highly developed and wealthy and some in the north are not (Longo, 2014). Scholars engaged in research in the GS prefer the term “Global North and South,” which consciously elides other distinctions that perpetuate the primacy of certain nation-states. For the purposes of this study, I refer to highly developed Western countries as GN and underserved, under-resourced non-Western countries as GS.
- Some participants’ survey responses were lightly proofed or edited for clarity.
ACKNOWLEDGEMENTS
The author would like to thank Dr. Biraj Pokhrel, Dr. Sushil Khanal, Sadikshya Upadhayay, and Hem Raj Neupane for their generous support throughout this study. The author would also like to thank Karla Saari Kitalong for her valuable advice and suggestions. Additional thanks to the journal editor, the special issue editors, and reviewers for their insightful comments and feedback to improve the manuscript.
ABOUT THE AUTHOR
Dr. Keshab Raj Acharya is a faculty member in the Department of Engineering Education at the University at Buffalo—SUNY, where he teaches courses related to technical and professional communication. He is available at keshab.acharya@gmail.com.
REFERENCES
Acharya, K. R. (2018). Usability for user empowerment: Promoting social justice and human rights through localized UX design. Proceedings of the 36th ACM International Conference on the Design of Communication. ACM. https://doi.org/10.1145/3233756.3233960
Acharya, K. R. (2019). Usability for social justice: Exploring the implementation of localization usability in Global North technology in the context of a Global South’s country. Journal of Technical Writing and Communication, 49(1), 6–32. https://doi.org/10.1177/0047281617735842
Adepoju, I. O., Albersen, B. J. A., De Brouwere, V., van Roosmalen, J., & Zweekhorst, M. (2017). mHealth for clinical decision-making in sub-Saharan Africa: A scoping review. JMIR mHealth and uHealth, 5(3). http://mhealth.jmir.org/2017/3/e38
Al Ayubi, S. U., Parmanto, B., Branch, R., & Ding, D. (2014). A persuasive and social mHealth application for physical activity: A usability and feasibility study. JMIR mHealth and uHealth, 2(2). https://doi.org/10.2196/mhealth.2902
Al-Ramahi, M., El-Gayar, O., & Liu, J. (2016). Discovering design principles for persuasive systems: A grounded theory and text mining approach. Proceedings of 2016 49th Hawaii International Conference on System Sciences (HICSS) (pp. 3074–3083). IEEE. https://doi.org/10.1109/HICSS.2016.387
Albrecht, U. V., Pramann, O., & von Jan, U. (2014) Synopsis for health apps: Transparency for trust and decision making. In M. Househ, E. Borycki, & A. Kushniruk (Eds.), Social media and mobile technologies for healthcare (pp. 94–108): IGI Global.
Alsswey, A. H., Al-Samarraie, H., El-Qirem, F. A., Alzahrani, A. I., & Alfarraj, O. (2020). Culture in the design of mHealth UI: An effort to increase acceptance among culturally specific groups. The Electronic Library, 38(2), 257–272. https://doi.org/10.1108/EL-04-2019-0097
Andrews, C., Burleson, D., Dunks, K., Elmore, K., Lambert, C. S., Oppegaard, B., Pohland, E. E., Saad, D., Scharer, J. S., Wery, R. L., Wesley, M., & Zobel, G. (2012). A new method in user-centered design: Collaborative prototype design process (CPDP). Journal of Technical Writing and Communication, 42(2), 123–142. https://doi.org/10.2190/TW.42.2.c
Apple Store Preview. (2021). Medscape. What’s new. Version history. Retrieved Jan. 31, 2022, from https://apps.apple.com/us/app/medscape/id321367289
Arduser, L. (2018). Impatient patients: A DIY usability approach in diabetes wearable technologies. Communication Design Quarterly, 5(4), 31–39. https://doi.org/10.1145/3188387.3188390
Armstrong, D., Gosling, A., Weinman, J., & Marteau, T. (1997). The place of inter-rater reliability in qualitative research: An empirical study. Sociology, 31(3), 597–606. https://doi.org/10.1177/0038038597031003015
Batova, T. (2010). Writing for the participants of international clinical trials: Law, ethics, and culture. Technical Communication, 57(3), 266–281.
Batova, T., & Clark, D. (2015). The complexities of globalized content management. Journal of Business and Technical Communication, 29(2), 221–235. https://doi.org/10.1177/1050651914562472
Baxter, K., Courage, C., & Caine, K. (2015). Understanding your users: A practical guide to user research methods (2nd ed.). Morgan Kaufmann.
Bhatta, R., Aryal, K., & Ellingsen, G. (2015). Opportunities and challenges of a rural-telemedicine program in Nepal. Journal of Nepal Health Research Council, 13(30), 149–153. https://doi.org/10.33314/jnhrc.v0i0.640
Boettger, R. K., & Palmer, L. A. (2010). Quantitative content analysis: Its use in technical communication. IEEE Transactions on Professional Communication, 53(4), 346–357. https://doi.org/10.1109/TPC.2010.2077450
Budiu, R. (2016). Mobile: Native apps, web apps, and hybrid apps. Retrieved from http://www.nngroup.com/articles/mobile-native-apps/
Cardinal, A., Gonzales, L., & Rose, E. (2020). Language and participation: Multilingual user experience design. Proceedings of the 38th ACM International Conference on Design of Communication. ACM. https://doi.org/10.1145/3380851.3416763
Chaudhary, R., Rabin, B., & Masum, P. (2019). Attitudes about the use of smartphones in medical education and practice in emergency department of tertiary care hospital. Journal of Health & Medical Informatics, 10(5), 1–6.
Creswell, J. (2009). Research design: Qualitative, quantitative, and mixed methods approaches (3rd ed.). Sage.
Dijkstra, J. J., Liebrand, W. B. G., & Timminga, E. (1998). Persuasiveness of expert systems. Behaviour and Information Technology, 17(3), 155–163. https://doi.org/10.1080/014492998119526
Dillman, D. A., Smyth, J. D., & Christian, L. M. (2014). Internet, phone, mail, and mixed-mode surveys: The tailored design method. John Wiley & Sons.
Dombrowski, L. (2017). Socially just design and engendering social change. Interactions, 24(4), 63–65. https://doi.org/10.1145/3085560
Ehn, P. (1992). Scandinavian design: On participation and skill. In P. S. Adler & T. A. Winograd (Eds.), Usability: Turning technologies into tools (pp. 96–132). Oxford University Press.
Esselink, B. (2000). A practical guide to localization. Benjamins.
Fink, A. (2017). How to conduct surveys: A step-by-step guide (6th ed.). Sage.
Fiordelli, M., Diviani, N., & Schulz, P. J. (2013). Mapping mHealth research: A decade of evolution. Journal of Medical Internet Research, 15(5). https://doi.org/10.2196/jmir.2430
Flick, U. (2018). An introduction to qualitative research (6th ed.). Sage.
Fogg, B. J. (2003). Persuasive technology: Using computers to change what we think and do. Morgan Kaufmann.
Fogg, B. J., Cuellar, G., & Danielson, D. (2009). Motivating, influencing, and persuading users: An introduction to captology. In A. Sear & J. A. Jacko (Eds.), The human-computer interaction handbook (pp. 109–172). CRC Press.
Gagnon, M. P., Ngangue, P., Payne-Gagnon, J., & Desmartis, M. (2016). m-Health adoption by healthcare professionals: A systematic review. Journal of American Medical Information Association, 23, 212–220. https://doi.org/10.1093/jamia/ocv052
Global mHealth Industry Landscape Overview 2020. (2020, November). Retrieved from https://www.biginnovationcentre.com/publications/page/3
Gonzales, L., & Zantjer, R. (2015). Translation as a user-localization practice. Technical Communication, 62(4), 271–284.
Google Play. (2022). Medscape. Retrieved Jan. 31, 2022, from https://play.google.com/store/apps/details?id=com.medscape.android
Granello, D. H., & Wheaton, J. E. (2004). Online data collection: Strategies for research. Journal of Counseling & Development, 82(4), 387–393. https://doi.org/10.1002/j.1556-6678.2004.tb00325.x
Gu, B., & Yu, M. (2016). East meets west on flat design: Convergence and divergence in Chinese and American user interface design. Technical Communication, 63(3), 231–247.
Hall, M., De Jong, M., & Steehouder, M. (2004). Cultural differences and usability evaluation: Individualistic and collectivistic participants compared. Technical Communication, 51(4), 489–503.
Hitt, A. (2018). Foregrounding accessibility through (inclusive) universal design in professional communication curricula. Business and Professional Communication Quarterly, 81(1), 52–65. https://doi.org/10.1177/2329490617739884
Hoft, N. L. (1995). International technical communication: How to export information about high technology. John Wiley & Sons.
Jones, N. N., & Williams, M. F. (2017). The social justice impact of plain language: A critical approach to plain-language analysis. IEEE Transactions on Professional Communication, 60(4), 412–429. https://doi.org/10.1109/TPC.2017.2762964
Jones, N. N., Moore, K. R., & Walton, R. (2016). Disrupting the past to disrupt the future: An antenarrative of technical communication. Technical Communication Quarterly, 25(4), 211–229. https://doi.org/10.1080/10572252.2016.1224655
Kennedy, K. (2018). Designing for human-machine collaboration: Smart hearing aids as wearable technologies. Communication Design Quarterly, 5(4), 40–51. https://doi.org/10.1145/3188387.3188391
Kirkscey, R. (2020). mHealth apps for older adults: A method for development and user experience design evaluation. Journal of Technical Writing and Communication, 51(2), 199–217. https://doi.org/10.1177/0047281620907939
Ladner, R. E. (2015). Design for user empowerment. Interactions, 22(2), 24–29. https://doi.org/10.1145/2723869
Lauer, C., & Brumberger, E. (2016). Technical communication as user experience in a broadening industry landscape. Technical Communication, 63(3), 248–264.
Lazakidou, A., & Iliopoulou, D. (2012). Useful applications of computers and smart mobile technologies in the health sector. Journal of Applied Medical Sciences, 1(1), 27–60.
Longo, B. (2014). Using social media for collective knowledge-making: Technical communication between the global north and south. Technical Communication Quarterly, 23(1), 22–34. https://doi.org/10.1080/10572252.2014.850846
Marcus, B., Weigelt, O., Hergert, J., Gurt, J., & Gelléri, P. (2017). The use of snowball sampling for multi-source organizational research: Some cause for concern. Personnel Psychology, 70(3), 635–673. https://doi.org/10.1111/peps.12169
Martin, S., Carrington, N., & Muncie, N. (2017). Promoting user advocacy to shift technical communication identity and value. Technical Communication, 64(4), 328–344.
Ming, L. C., Hameed, M. A., Lee, D. D., Apidi, N. A., Lai, P. S. M., Hadi, M. A., Al-Worafi, Y. M. A., & Khan, T. M. (2016). Use of medical mobile applications among hospital pharmacists in Malaysia. Therapeutic Innovation & Regulatory Science, 50(4), 419–426. https://doi.org/10.1177/2168479015624732
Naderifar, M., Goli, H., & Ghaljaie, F. (2017). Snowball sampling: A purposeful method of sampling in qualitative research. Strides in Development of Medical Education, 14(3), 1–4. https://doi.org/10.5812/sdme.67670
Odeh, L. E. (2010). A comparative analysis of Global North and Global South economies. Journal of Sustainable Development in Africa, 12(3), 338–348.
Ohno-Machado, L. (2015). Tailoring informatics interventions to patients and healthcare providers. Journal of the American Medical Informatics Association, 22(4), 747. https://doi.org/10.1093/jamia/ocv075
Oinas-Kukkonen, H, & Harjumaa, M. (2018). Persuasive systems design: Key issues, process, and system features. In M. Howlett & I. Mukherjee (Eds.). Routledge handbook of policy design (pp. 87–105). Routledge.
Opel, D. (2014). Social justice in technologies of prenatal care: Toward a user centered approach to technical communication in home pregnancy testing. Proceedings of the 32nd ACM International Conference on The Design of Communication. ACM. https://doi.org/10.1145/2666216.2666223
Osei, E., & Mashamba-Thompson, T. P. (2021). Mobile health applications for disease screening and treatment support in low-and middle-income countries: A narrative review. Heliyon, 7(3). https://doi.org/10.1016/j.heliyon.2021.e06639
Oswal, S. K. (2019). Breaking the exclusionary boundary between user experience and access: Steps toward making UX inclusive of users with disabilities. Proceedings of the 37th ACM International Conference on the Design of Communication. ACM. https://doi.org/10.1145/3328020.3353957
Phillips, A., & Thornbory, G. (2014). Apps for health professionals. Occupational Health & Wellbeing, 66(4), 27.
Pokhrel, P., Karmacharya, R., Taylor Salisbury, T., Carswell, K., Kohrt, B. A., Jordans, M. J. D., Lempp, H., Thornicroft, G., & Luitel, N. P. (2021). Perception of healthcare workers on mobile app-based clinical guideline for the detection and treatment of mental health problems in primary care: A qualitative study in Nepal. BMC Medical Informatics and Decision Making, 21(1), 1–12. https://doi.org/10.1186/s12911-021-01386-0
Rebedew, D. (2018). Six mobile apps to make prescribing easier. Family Practice Management, 25(6), 11–16.
Rose, E. J. (2016). Design as advocacy: Using a human-centered approach to investigate the needs of vulnerable populations. Journal of Technical Writing and Communication, 46(4), 427–445. http://dx.doi.org/10.1177/0047281616653494
Rose, E. J., Racadio, R., Wong, K., Nguyen, S., Kim, J., & Zahler, A. (2017). Community-based user experience: Evaluating the usability of health insurance information with immigrant patients. IEEE Transactions on Professional Communication, 60(2), 214–231. https://doi.org/10.1109/TPC.2017.2656698
Roth, V. J. (2014). The mHealth conundrum: Smartphones & mobile apps—how much FDA medical device regulation is required? North Carolina Journal of Law & Technology, 15(3), 359–429.
Roy, D. (2013). Toward experience design: The changing face of technical communication. Connexions • International Professional Communication Journal, 1(1), 111–118.
Saru, E. H., & Wojahn, P. (2020). “Glocalization” of health information: Considering design factors for mobile technologies in Malaysia. Journal of Technical Writing and Communication, 50(2), 187–206. https://doi.org/10.1177/0047281620906131
Sauer, G. (2018). Applying usability and user experience within academic contexts: Why progress remains slow. Technical Communication Quarterly, 27(4), 362–371. https://doi.org/10.1080/10572252.2018.1521637
Sezgin, E., Özkan-Yildirim, S., & Yildirim, S. (2017). Investigation of physicians’ awareness and use of mHealth apps: A mixed method study. Health Policy and Technology, 6(3), 251–267. https://doi.org/10.1016/j.hlpt.2017.07.007
Shati, A. (2020). mHealth applications developed by the Ministry of Health for public users in KSA: A persuasive systems design evaluation. Health Informatics International Journal, 9(1), 1–13. https://doi.org/10.5121/hiij.2020.101
Spinuzzi, C. (2005). The methodology of participatory design. Technical Communication, 52(2), 163–174.
St.Amant, K. (2015). Introduction to the special issue: Cultural considerations for communication design: Integrating ideas of culture, communication, and context into user experience design. Communication Design Quarterly, 4(1), 6–22. https://doi.org/10.1145/2875501.2875502
St.Amant, K. (2017a). The cultural context of care in international communication design: A heuristic for addressing usability in international health and medical communication. Communication Design Quarterly, 5(2), 62–70. https://doi.org/10.1145/3131201.3131207
St.Amant, K. (2017b). Of scripts and prototypes: A two-part approach to user experience design for international contexts. Technical Communication, 64(2), 113–125.
St.Amant, K. (2021). Creating scripts for crisis communication: COVID-19 and beyond. Journal of Business and Technical Communication, 35(1), 126–133. https://doi.org/10.1177/1050651920959191
St. Germaine-McDaniel, N. (2010). Technical communication in the health fields: Executive Order 13166 and its impact on translation and localization. Technical Communication, 57(3), 251–265.
Stake, R. E. (1995). The art of case study research. Sage.
Strecher, V. J. (1999). Computer-tailored smoking cessation materials: A review and discussion. Patient Education & Counseling, 36(2), 107–117. https://doi.org/10.1016/S0738-3991(98)00128-1
Sun, H. (2012). Cross-cultural technology design: Creating culture-sensitive technology for local users. Oxford University Press.
Sun, H. (2020). Global social media design: Bridging differences across cultures. Oxford University Press.
Sun, H., & Getto, G. (Eds.) (2017). Localizing user experience: Strategies, practices, and techniques for culturally sensitive design [Special section]. Technical Communication, 64(2), 89–94.
Wallace, S., Clark, M., & White, J. (2012). It’s on my iPhone: Attitudes to the use of mobile computing devices in medical education, a mixed-methods study. BMJ Open, 2(4). http://dx.doi.org/10.1136/bmjopen-2012-001099
Walton, R. (2016). Supporting human dignity and human rights: A call to adopt the first principle of human-centered design. Journal of Technical Writing and Communication, 46(4), 402–426. https://doi.org/10.1177/0047281616653496
WebMD LLC. (2022, November). Medscape. Retrieved from https://www.medscape.com/public/medscapeapp
Welhausen, C. A., & Bivens, K. M. (2021). mHealth apps and usability: Using user-generated content to explore users’ experiences with a civilian first responder app. Technical Communication, 68(3), 97–112.
Wright, K. B. (2005). Researching Internet-based populations: Advantages and disadvantages of online survey research, online questionnaire authoring software packages, and web survey services. Journal of Computer-Mediated Communication, 10(3). https://doi.org/10.1111/j.1083-6101.2005.tb00259.x
Zhang, J., Johnson, T. R., Patel, V. L., Paige, D. L., & Kubose, T. (2003). Using usability heuristics to evaluate patient safety of medical devices. Journal of Biomedical Informatics, 36(1–2), 23–30. https://doi.org/10.1016/S1532-0464(03)00060-1
Zhu, P., & St.Amant, K. (2007). Taking traditional Chinese medicine international and online: An examination of the cultural rhetorical factors affecting American perceptions of Chinese-created Web sites. Technical Communication, 54(2), 171–186.
APPENDIX
Sample Survey Questions
- What are your purposes of using mHealth apps? (Please select all that apply)
- To improve the performance of healthcare
- To support patient needs and expectations
- To find information for effective patient treatment
- To provide immediate care and health support
- To make quick decisions during critical care situations
- To find reliable medical and health information
- Other (Please specify)
- How often do you use mHealth apps other than the Medscape app?
- Always
- Very often
- Sometimes
- Rarely
- How often do you use the Medscape app?
- many times a day
- once a day
- many times a week
- once or twice a week
- once a month
- How long have you been using the Medscape app?
- Less than 1 month
- More than 1 month
- How easy was it to install and operate the app on your device?
- Very easy
- Easy
- Neither difficult nor easy
- Difficult
- Very difficult
- Why do you want to use the Medscape app? (Please select all that apply)
- o Because the app is free to download
- Because it is well designed and easy to use
- Because my colleagues and many other medical professionals use it in my country
- Because I learned about it from my fellow medical and healthcare practitioners in my workplace
- Other (please specify)
- The information in the Medscape app is well organized or designed, so I can easily find and understand what I need.
- Strongly agree
- Somewhat agree
- Neither agree nor disagree
- Somewhat disagree
- Strongly disagree
- Is the Medscape app designed and developed to meet your needs and expectations?
- Yes, it is designed and developed to meet the needs and expectations of users like myself.
- Yes, it is designed and developed to meet the needs and expectations of users, but it is always not easy to use the app.
- No, it is not designed and developed to meet the needs and expectations of users like myself.
- If not, what should be done so that the app meets your needs and expectations?
- What do you prefer to use?
- Medscape app
- Medscape website
- Both
- If you prefer the Medscape website to the app, why?
- The information provided in the application is very reliable.
- Strongly agree
- Somewhat agree
- Neither agree nor disagree
- Somewhat disagree
- Strongly disagree
- How often the app crashes or causes problems on your devices?
- Always
- Very often
- Sometimes
- Rarely
- Never
- I can use the app even when the internet connection is poor or not available.
- Strongly agree
- Somewhat agree
- Neither agree nor disagree
- Somewhat disagree
- Strongly disagree
- The app has improved my access to healthcare information, medical news, medical education, and consultations with experts.
- Strongly agree
- Somewhat agree
- Neither agree nor disagree
- Somewhat disagree
- Strongly disagree
- How satisfied are you with the app?
- Extremely satisfied
- Somewhat satisfied
- Neither satisfied nor dissatisfied
- Somewhat dissatisfied
- Extremely dissatisfied
- How likely are you to recommend the app to a friend or colleague?
- Extremely likely
- Somewhat likely
- Neither likely nor unlikely
- Somewhat unlikely
- Extremely unlikely
- What confuses or annoys you about the app?
- What should be done to make the app more usable, accessible, and reliable for users?
- What other mHealth apps do you use?