By Gaya Gamhewage, Richelle George, Heini Utunen
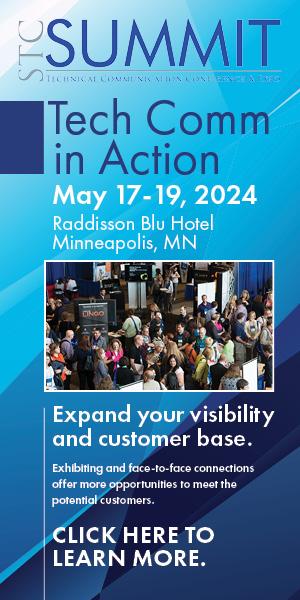
According to the World Health Organization (WHO), risk communication is defined as “the real-time exchange of information, advice and opinions between experts, officials and the communities affected by a hazard.” Risk communication is about more than just a one-way exchange of information from experts and officials to affected communities. It is characterized by the reciprocal exchange of information and communication between public health officials and affected communities, as shown in Figure 1.
For any outbreak (including an influenza epidemic) an early, proactive, and rapid public health response provides the greatest opportunity to limit morbidity and mortality and to reduce the damage caused to people’s societal and economic well-being. Public health risk communication is a key component of this response.
During the 1970s, Paul Slovic researched how people perceive risk. His research found that the general public is less likely to be concerned about health risks that are voluntary, familiar, controllable, fair, non-fatal, diffuse, and slow-acting (Slovic et al. 1979). For example, a person may voluntarily decide to get into a car and not wear a seatbelt, despite the risk involved. Many people decide that it is okay to have unsafe sex or run across a crowded road. These are risks that people are willing to take precisely because they take them voluntarily.
Slovic’s research found that the opposite is true for risks that are perceived to be significant. These risks are involuntary, obligatory, unfamiliar, uncontrollable, unfair, acute, fatal, and quickly traverse geographical space and time (Slovic et al. 1979). Ebola or a radio-nuclear disaster are examples of the kind of risks that, for these reasons, engender concern among the general public. Though these tendencies might differ in different communities, Slovic’s work reflects some general factors that determine how people perceive risk. Understanding the critical influence of perception on how people behave and whether they follow an expert’s advice is crucial for public health professionals.
Perception is rooted in the subconscious and is often illogical. An expert might offer logical, evidence-based, scientific information, but this might have little influence over people’s perceptions, which are developed in a different part of the brain (Gifford 1986). This part of the brain is influenced by culture, colored by emotions, and not always expressed verbally. While some say that epidemiologists and scientists frame scientific risk, laypeople create and experience lived risk. The expert might think that people are agreeing with advice given to them. The perception of risk, however, will show only in people’s behavior. As a result, it is key that experts and scientists (particularly bio-medical scientists) acknowledge other kinds of science, including behavioral and social science—the study of emotions, attitudes, beliefs, and customs and how these affect the communication of risk.
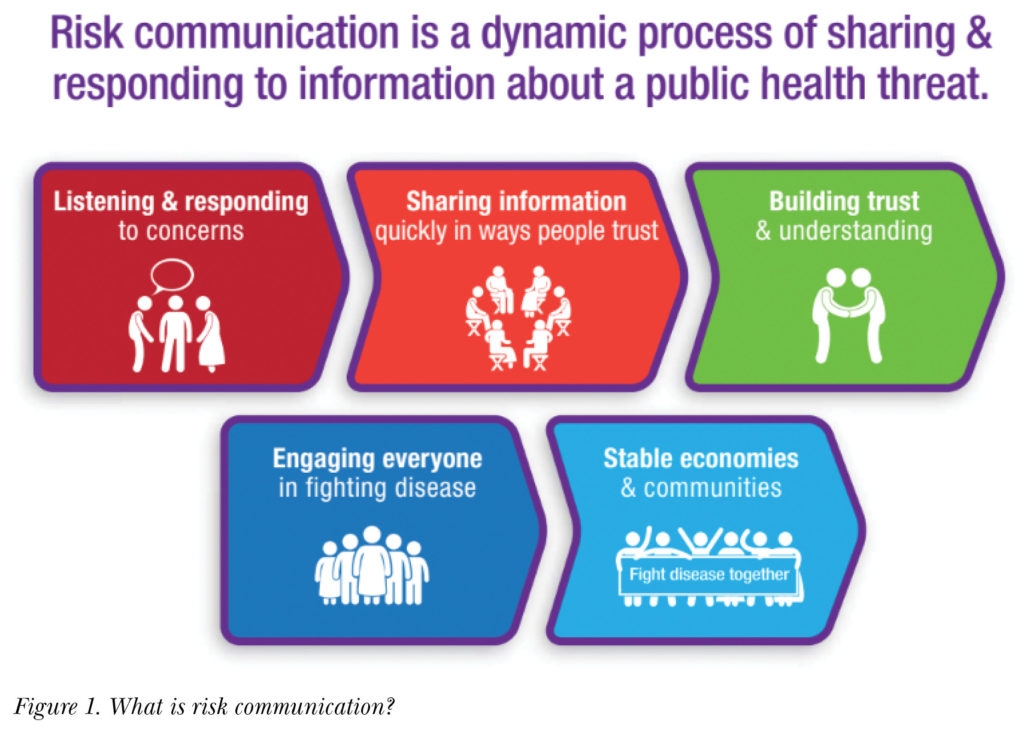
Much research has been done into what makes good risk communication. For the World Health Organization, Ministries of Health, and other public health organizations, technical information is a key part of effective risk communication. In addition to technical information, however, there are four other components of risk communication, as shown in Figure 2. Risk communication:
- must address the values of affected communities
- is dependent on the trust people have in authorities and experts
- depends on the credibility of the person or agency communicating the risk
- must incorporate expressions of caring.
Though these five components make up effective risk communication, one component is more important than the others: trust. The trust people have in authorities, experts, and organizations is, by far, the greatest ingredient for effective risk communication. A public health expert might have accurate, factual information, but if people do not trust or believe them, people are unlikely to follow their advice. Remembering this is critical to effective risk communication.
Many strategies and tactics make up risk communication—it should not be limited to just public or media communication and social media. Risk communication also includes massive awareness initiatives, including social mobilization, community engagement, social behavior change communication, and political communication. Effective risk communication will apply most of these strategies, along with dynamic listening in interpersonal communication, as shown in Figure 3, to convey messages to key audiences.
 The History Behind Risk Communication—and Lessons Learned
The History Behind Risk Communication—and Lessons Learned
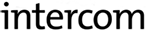
How risk is communicated has evolved over the last one hundred years. Figure 4 shows examples of recent epidemics.
In the early 20th century, Spanish influenza killed millions of people. During this time, there was unprecedented death and fear, partly because the public health tools of today didn’t exist then.
In the 21st century, which began with new diseases like SARS, public health experts’ focus on personal protection resulted in people resorting to using masks and body thermal detectors being installed in airports. SARS caused significant disruption to lives and livelihoods, as well as large-scale economic damage. Because of this, an understanding emerged that health risks and epidemics are much more than a health issue and that they have social and economic repercussions.
Epidemics in the present day are even more complicated due to high-speed travel, international trade, and a globalized world. Moreover, the contemporary world is characterized by information technology that has proliferated so widely across the globe that more than half of all people have access to the internet (Digital Information World 2018), and more people today have access to telephones than safe toilets (UN News 2013). More than half of the world’s population currently lives in densely populated cities. These factors, combined, result in increased health risks, not only in relation to the emergence of diseases but the rapid amplification of these diseases into epidemics and pandemics.
Public health practitioners have learned many lessons over the years. From the outbreak of SARS in 2003, they learned that disease epidemics are much more than health-related issues. They learned that even wealthy countries can become paralyzed by disease outbreaks and that economies may suffer for many years. Through SARS, public health officials witnessed the way that a disease can be exported to many parts of the world through travel. Though SARS was a milder pandemic than the world had anticipated, several hundred thousand people died. In addition, there was a lack of trust in public health institutions and many rumors and conspiracy theories about the origin of the disease abounded.
In 2012, during the spread of Middle East respiratory syndrome coronavirus (MERS-CoV) in the Eastern Mediterranean and Saudi Arabia, public health officials witnessed a virus rapidly amplify in hospitals and other care-giving facilities.
Beginning in 2014, the outbreak of Ebola virus disease in West Africa continued for two years and shook the world. Public health practitioners learned a great deal about risk communication during the Ebola outbreak. For example, they learned that sending out messages and putting out posters does not constitute effective risk communication and that engagement with communities—understanding what they believe and what is important to them—is key. The Ebola outbreak in West Africa revolutionized all of emergency response, and one of the biggest lessons learned was about risk communication and other social science interventions.
The year 2015 saw yet another outbreak of MERS-CoV, this time in South Korea. One infected patient introduced the disease to a new part of the world, where it was amplified in hospitals, causing many deaths.
From 2015 to 2016, Zika spread across the Americas. This outbreak provided a valuable learning opportunity for public health officials regarding the challenging topics that require specialised risk communication, such as issues surrounding women’s reproductive health.
Due to the 2016 outbreak of Yellow Fever in Africa, public health practitioners had to learn how to communicate health-related messages about new formulations of vaccines, while at the same time vaccinating thirty to forty million people in a short period. Risk communication and social science interventions played a significant role in these activities.
Step by Step: Communicating Risk for an Influenza Outbreak
From these experiences, public health organizations have significantly improved their practice. Over the last twenty to thirty years, they have learned that every agency and individual involved in risk communication must create and maintain trust. Moreover, it has become clear that public health officials must acknowledge and communicate risk even when they don’t necessarily have all the facts—and be honest about it. Communicating amid uncertainty requires skill and courage, but if it is not done, the result will be misinformation, rumors, and a lack of trust.
Effective risk communication also requires coordination. An official might be working in a lab, on a surveillance team, or as part of a response team, but there may be many other players with  whom they must coordinate information sharing and risk communication. Depending on the outbreak, this might include the animal health sector. Public health practitioners must be quick and transparent in their risk communication, especially near the start of an outbreak. If public health practitioners are not the first to communicate risk during an outbreak, they will spend the rest of the outbreak trying to correct misinformation.
whom they must coordinate information sharing and risk communication. Depending on the outbreak, this might include the animal health sector. Public health practitioners must be quick and transparent in their risk communication, especially near the start of an outbreak. If public health practitioners are not the first to communicate risk during an outbreak, they will spend the rest of the outbreak trying to correct misinformation.
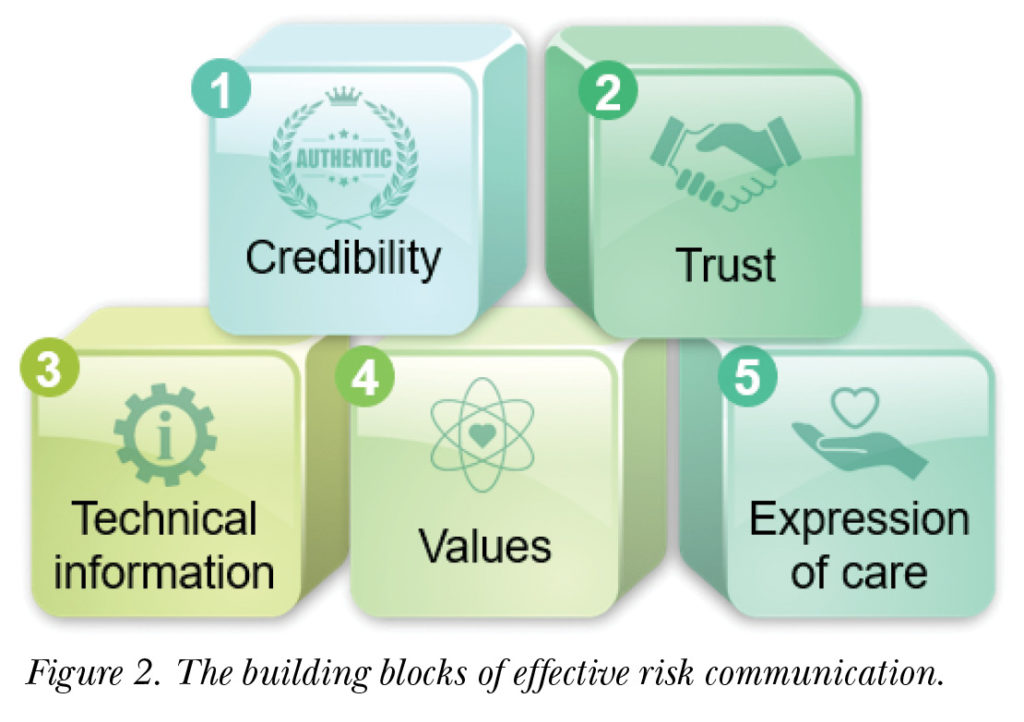
The expertise of the WHO lies in the central cog of the wheel in Figure 5—biomedical expertise. The WHO is an evidence-based, science-based, bio-medical organization. As a result of organizational reform, it has also become operational. To adapt, the organization must integrate social science approaches, including risk communication, into its biomedical and operational work. In integrating these, the organization will have a much better chance of detecting and responding to outbreaks, epidemics, and pandemics.
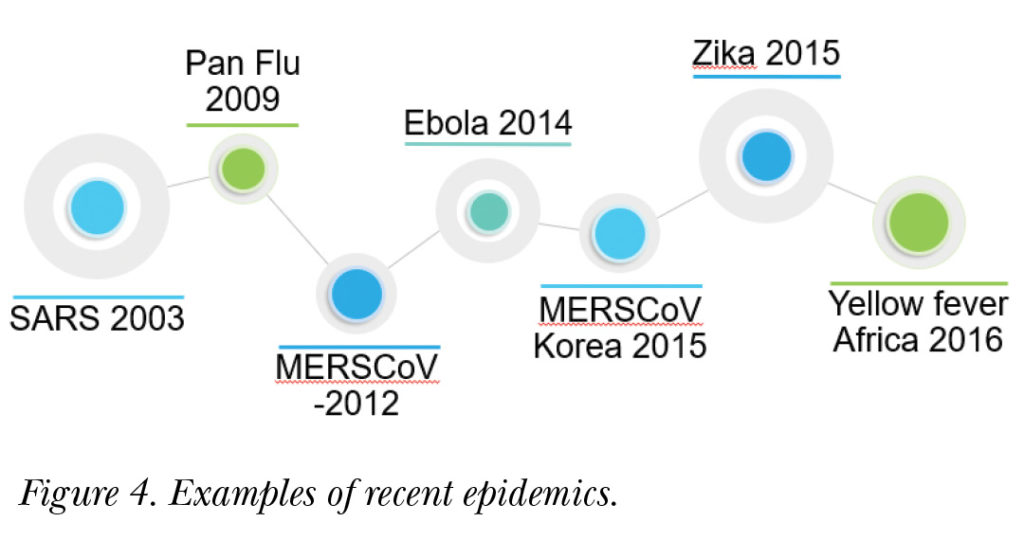
The opportunities for risk communication exist across a broad spectrum of situations, as shown in the influenza example in Figure 6, from the emergence of zoonotic disease to preparedness and early detection, from managing the progress of an outbreak and its localized transmission to containment, mitigation, and control in the case of an epidemic or pandemic. For each stage in this process, there are different risk communication strategies, tactics, and other tools that must be employed.
Communicating Risk for an Outbreak of Zoonotic Influenza
To respond to an outbreak of zoonotic influenza, public health practitioners must ask:
- Which animals are risk factors in the spread of the disease?
- What is the economic and cultural context of the outbreak?
- Who should be responsible, in this context, for delivering public health-related messages and when should they relay them?
Questions like these are only examples of those that should be asked at the onset of an outbreak of zoonotic influenza. During such an outbreak, the collaboration between the animal, human, food, trade, and livestock sectors must be well coordinated. In the past, at the global level, the WHO has worked closely with the World Organisation for Animal Health and has also engaged in joint risk communication activities with actors at the local level.
Communicating Risk for an Outbreak of Seasonal Influenza
For seasonal influenza outbreaks, public health practitioners must target messages toward communities most at risk. They must ask questions like:
- What is the prevailing perception of the outbreak among affected communities?
- What is the current use of pharmaceutical and non-pharmaceutical interventions?
- Is the flu vaccine used in the affected country?
- What are people’s perceptions of non-pharmaceutical interventions?
- Are people aware of the benefits of regular hand-washing or proper respiratory etiquette, like coughing and sneezing into one’s sleeve?
- Are people aware of the benefits of social distancing? If not, who would they trust to communicate risk to them?
Communicating Risk for an Outbreak of Pandemic Influenza
An outbreak of pandemic influenza can be devastating. Here, public health officials must ask:
- Who is most at risk?
- What are the prevailing perceptions that surround the outbreak?
- Will people be complacent because the last outbreak of pandemic influenza, in 2009, was relatively mild?
Public health officials might also be faced with vaccine hesitancy from those who do not trust the vaccine or perhaps don’t understand how it is developed. According to the WHO’s Regional Office for Europe (EURO), the reasons for vaccine hesitancy vary widely across the member states. Effectively responding to vaccine hesitancy requires an understanding of the relevant “complex web of social issues” and a systemic approach to grasping the impact of culture on perceptions of health and well-being (EURO 2018). In such situations, public health practitioners must ask:
- What is the current use of vaccines, antivirals, and non-pharmaceutical interventions in the affected areas?
- Who is trusted to communicate risk or give advice in this situation?
- Are the concerns of the general public being listened to?
These are some of the questions that public health practitioners should ask during any of the three hypothetical scenarios described in this article.
Conclusion
The basic principles to remember for risk communication are:
- First, create and maintain trust.
- Second, understand, listen to, and address the perceptions and concerns of at-risk populations.
- Third, communicate frequently, and be proactive and transparent.
The major challenge concerning emergency risk communication is building and maintaining trust. One-way, evidence-based communication inhibits effective engagement of communities. People might politely listen, but that doesn’t guarantee that they will follow the advice given. As a result, community engagement with affected communities must be at the center of risk communication. Part of a risk communicator’s job is ensuring that community influencers and leaders engage with their messages.
Translational communication—presenting the scientific, epidemiological, and laboratory work in a format and language that laypeople and affected communities can understand—is also important for effective risk communication. It is key to avoid the assumption that senior officials and decision-makers might understand this information. Public health officials must be aware of their jargon and terminology and the fact that the audience might not always express that they don’t understand.
Furthermore, public health work for pandemic influenza requires stakeholder coordination and community engagement, and most importantly, dynamic listening. Tools, such as social media surveillance, partner stakeholder feedback, anthropology, and knowledge-attitude practice studies, may be used. Public health practitioners engaged in risk communication must be aware of these tools and be able to involve and assist the experts who do this work.
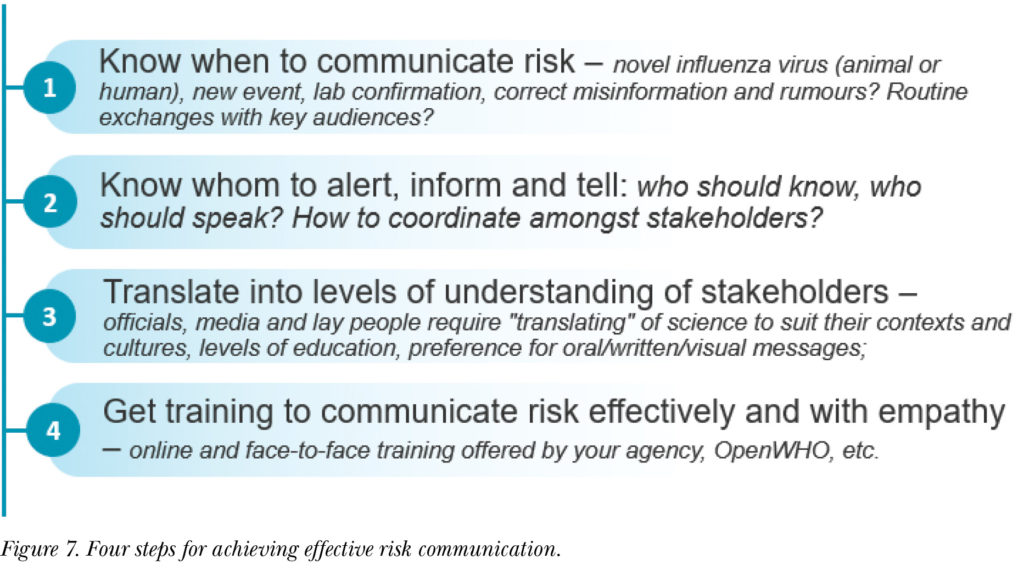
All public health experts must understand risk communication and their role in communicating risk. The four steps for risk communication, as shown in Figure 7, are to:
- Know when to communicate risk.
- Know who is most appropriate to communicate risk to the public and understand who your audience is.
- Engage in translational communication.
- Share information appropriately between relevant stakeholders, officials, media, and laypeople.
Don’t forget to translate materials into the local languages of affected communities. Translational communication isn’t just about language but also accounting for the health belief model (HBM) of affected communities.
To be prepared, risk communication training should begin as soon as possible before an outbreak. To assist with this, the WHO can offer online and face-to-face training in risk communication. The WHO has also developed materials for specific outbreaks, such as a Zika app, which contains all of the relevant information regarding Zika. The WHO’s Learning and Capacity Development Unit has also developed an online
knowledge-transfer platform called OpenWHO.org, which includes courses on all aspects of health emergencies, including risk communication.
Ultimately, the primary lesson public health officials have learned over the past few decades is to communicate risk before it’s too late. Unfortunately, the image of Ebola that has lingered in the public conscience is one characterized by the unknown, a lack of community engagement, and poor risk communication around safe and dignified burials. Risk communication must start before an epidemic begins if we are to prevent such a situation from arising again. Every public health professional has a role in this.
GAYA GAMHEWAGE, PHD, (gamhewageg@who.int) is Head of Learning and Capacity Development unit of WHO’s Health Emergencies Programme, based at WHO Headquarters in Geneva, Switzerland. A medical doctor by training, Dr. Gamhewage has more than two decades of experience in public health, including 18 years at WHO. She has obtained master’s degrees in public health and international policy making. She led the development of the WHO’s first-ever, evidence-based guideline on communicating risk in health emergencies.
HEINI UTUNEN (utunenh@who.int) is a Technical Officer in the Learning and Capacity Development unit of WHO’s Health Emergencies Programme, based at WHO Headquarters in Geneva, Switzerland. She holds degrees in information studies and political science and is an expert in capacity building, knowledge transfer, and simulation exercise management. She leads the effort to operationalize, and manages all of the online learning for, WHO’s health emergencies work.
RICHELLE GEORGE (georger@who.int) is a Consultant in the Learning and Capacity Development unit in WHO’s Health Emergencies Programme. She holds a degree in social anthropology. Her interests include the social determinants of health, health equity, and the role of the social sciences in optimizing health interventions during emergencies.
Resources
Digital Information World. 2018. “Digital in 2018: Essential Insights into the Internet, Social Media, Mobile, And Ecommerce Use Around the World.” Published 24 July 2018. https://www.digitalinformationworld.com/2018/07/global-internet-stats-infographic.html.
Gifford. S. 1986. “The Meaning of Lumps: A Case Study of the Ambiguities of Risk.” In Anthropology and Epidemiology, edited by Craig R. Janes, Ron Stall, and Sandra M. Gifford, 213–246. New York: Springer.
Slovic, Paul, Baruch Fischhoff, and Sarah Lichtenstein. 1979. “Rating the Risks.” Environment: Science and Policy for Sustainable Development 21.3 (April): 14–39.
UN News. 2013. “Deputy UN chief calls for urgent action to tackle the global sanitation crisis.” Accessed 11 January 2020. https://news.un.org/en/story/2013/03/435102-deputy-un-chief-calls-urgent-action-tackle-global-sanitation-crisis.
World Health Organization. n.d. Risk Communication for Influenza Events. Accessed February 25, 2020. https://openwho.org/courses/risk-communication-influenza.
World Health Organization. 2016. WHO Zika App. https://itunes.apple.com/us/app/who-zika-app/id1090088404?mt=8; https://play.google.com/store/apps/details?id=com.universaldoctor.zika&hl=en.
World Health Organization Europe. 2018. “106th Global Health Histories seminar: Vaccine Hesitancy—Why Do Some People Not Vaccinate?” Published 23 July 2018. http://www.euro.who.int/en/data-and-evidence/news/news/2018/7/106th-global-health-histories-seminar-vaccine-hesitancy.-why-do-some-
people-not-vaccinate.